Type 2 Diabetes
Get valuable insights into Type 2 Diabetes, including its causes, symptoms, prevention strategies, and treatment options, while also learning about how you can lower the cost of the medications used to treat Type 2 Diabetes.

MEDICAL INFORMATION
Type 2 Diabetes Key Facts
Related Medications
What is the definition of type 2 diabetes?
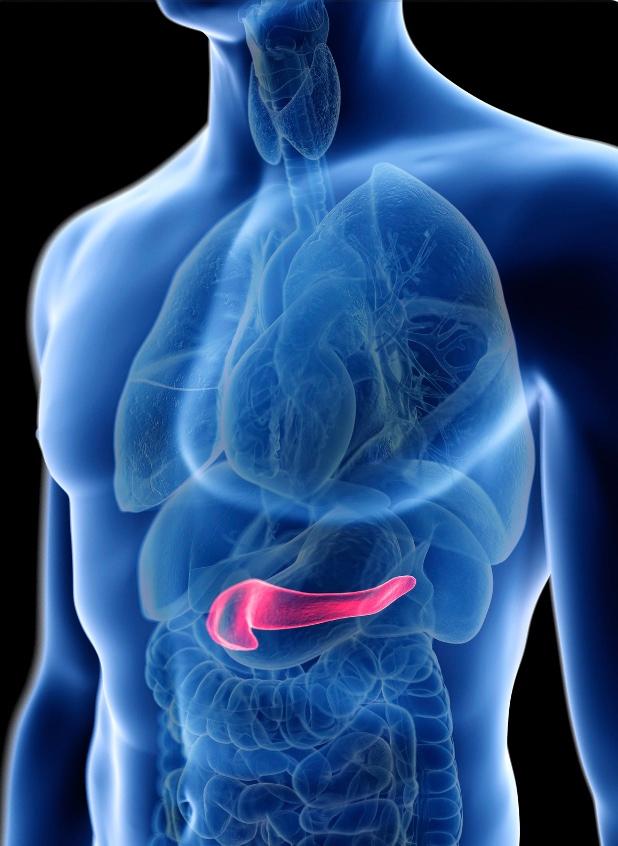
Type 2 diabetes, also known as non-insulin-dependent diabetes, occurs when the body becomes resistant to the effects of insulin or the pancreas fails to produce enough insulin to regulate blood sugar levels. Insulin is a hormone that helps transport glucose from the bloodstream into cells for energy.
What are the causes and risk factors of type 2 diabetes?
Type 2 diabetes, which used to be known as adult-onset diabetes, is a complex condition influenced by various causes and risk factors. While the exact cause is not fully understood, several factors contribute to its onset and development. Here are some of the known causes and risk factors:
Obesity and overweight
Excess body weight, especially around the waist, increases the risk of type 2 diabetes.
Lack of physical activity
Leading a sedentary lifestyle and not engaging in regular exercise can increase the risk of developing diabetes.
Unhealthy diet
Consuming a diet high in processed foods, sugary beverages, unhealthy fats, and low in fruits, vegetables, and whole grains can contribute to the development of type 2 diabetes.
Family history and genetics
Having a close family member with type 2 diabetes increases the risk. Genetic factors can influence how the body processes glucose.
Age
The risk of type 2 diabetes increases with age, especially after the age of 45.
Ethnicity
Certain ethnic groups, such as African Americans, Hispanic/Latino Americans, Native Americans, and Asian Americans, have a higher risk of developing type 2 diabetes.
Gestational diabetes
Women who have had gestational diabetes during pregnancy are at higher risk of developing type 2 diabetes later in life.
Polycystic ovary syndrome (PCOS)
Women with PCOS, a hormonal disorder, have a higher risk of developing type 2 diabetes.
High blood pressure and cardiovascular disease
These conditions are often associated with type 2 diabetes and share common risk factors.
Smoking
Smoking can increase the risk of developing type 2 diabetes and other health complications.
It’s important to note that having one or more of these risk factors doesn’t necessarily mean a person will develop type 2 diabetes. Lifestyle modifications, such as maintaining a healthy weight, engaging in regular physical activity, and adopting a balanced diet, can significantly reduce the risk of developing the condition. Regular check-ups and early detection are also crucial for timely intervention and management of diabetes.
What are the symptoms of type 2 diabetes?
Type 2 diabetes often develops gradually, and some individuals may not experience noticeable symptoms initially. However, as the condition progresses, the following symptoms of diabetes may occur:
Frequent urination
Increased need to urinate, especially during the night (nocturia).
Excessive thirst
Feeling extremely thirsty and having an unquenchable desire to drink fluids.
Unexplained weight loss or weight gain
Sudden weight loss, despite increased appetite, can occur in some cases. Conversely, weight gain may also be observed.
Fatigue
Feeling tired, weak, and lacking energy, even after adequate rest.
Blurred vision
Vision may become blurry or impaired, affecting the ability to see clearly.
Slow wound healing
Cuts, sores, or wounds take longer to heal than usual.
Frequent infections
Recurring infections, particularly urinary tract infections (UTIs) and yeast infections, may be experienced.
Tingling or numbness
Nerve damage caused by diabetes, known as diabetic neuropathy, can lead to tingling, numbness, or a burning sensation in the hands, feet, or legs.
Increased hunger
Persistent feelings of hunger, even after eating, may be experienced.
Darkened skin patches
Areas of the skin, particularly in the neck, armpits, or groin, may develop a velvety texture and appear darker.
It’s important to note that some individuals may not experience any symptoms or may have mild symptoms that go unnoticed. Regular check-ups and blood tests are crucial for diagnosing diabetes, especially in individuals with risk factors or a family history of the disease. If you suspect you may have type 2 diabetes or are experiencing any concerning symptoms, it’s important to consult with a healthcare professional for an accurate diagnosis and appropriate management.
How is type 2 diabetes diagnosed?
The diagnosis of type 2 diabetes involves several steps and assessments. Here’s an overview of the typical diagnostic process:
Symptom evaluation
If you have symptoms suggestive of diabetes, such as frequent urination, excessive thirst, unexplained weight loss or gain, fatigue, or others mentioned earlier, your healthcare provider will evaluate and discuss your symptoms in detail.
Medical history
Your doctor will inquire about your medical history, including any previous instances of high blood sugar, gestational diabetes (if applicable), family history of diabetes, and other relevant information.
Physical examination
A physical examination may be conducted to check for signs of diabetes-related complications and evaluate your overall health.
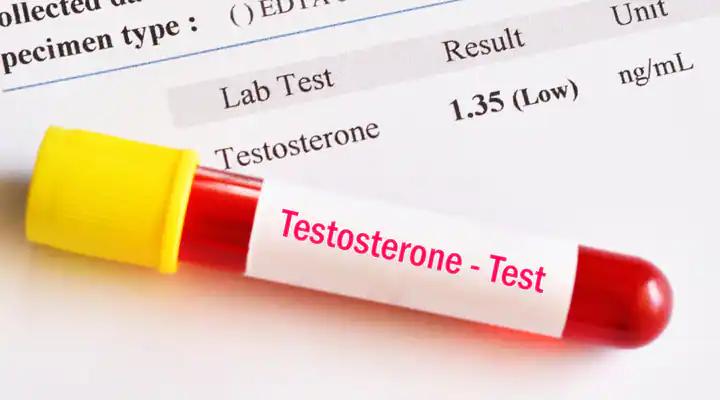
Blood tests
Blood tests are essential for diagnosing diabetes. The following tests are commonly performed:
- Fasting plasma glucose (FPG) test: This test measures your blood sugar level after an overnight fast. A value of 126 milligrams per deciliter (mg/dL) or higher on two separate occasions typically indicates diabetes
- Oral glucose tolerance test (OGTT): This test involves drinking a glucose solution, and then blood sugar levels are measured two hours later. A result of 200 mg/dL or higher confirms diabetes
- Glycated hemoglobin (A1C) test: This test provides an average blood sugar level over the past two to three months. An A1C level of 6.5% or higher usually indicates diabetes
Additional tests
Depending on the situation, your doctor may order additional tests to evaluate your overall health and check for potential complications of diabetes. These may include kidney function tests, lipid profile (cholesterol levels), liver function tests, and more.
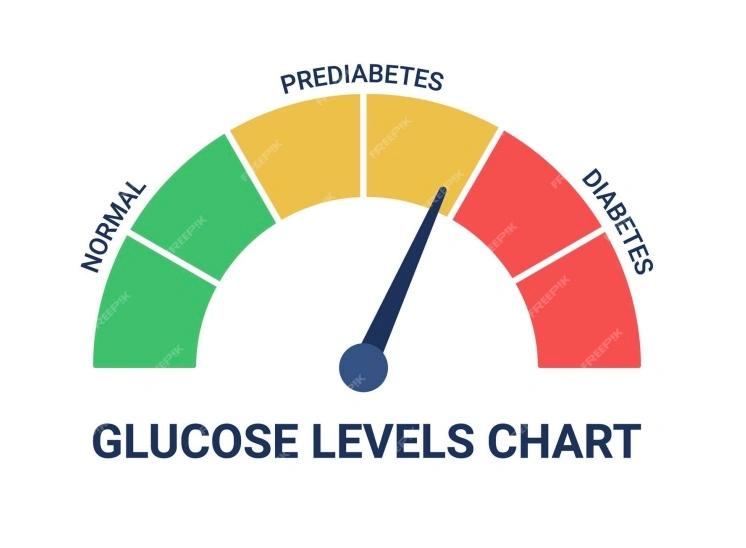
What is pre-diabetes?
Prediabetes is a health condition where blood sugar levels are higher than normal, but not high enough to be classified as type 2 diabetes. It’s often a precursor to type 2 diabetes, although it doesn’t always progress to this condition. Approximately 96 million American adults, which equates to more than 1 in 3 adults, have prediabetes.
Prediabetes is generally asymptomatic, meaning most people with prediabetes don’t experience noticeable symptoms. Because of this, many individuals may not realize they have the condition.
Risk factors for prediabetes include:
- being overweight
- being 45 years or older
- having a family history of type 2 diabetes
- having a history of gestational diabetes or giving birth to a baby who weighed more than 9 pounds
- not being physically active
- having polycystic ovary syndrome
If you have prediabetes, lifestyle changes such as adopting a healthy diet, increasing physical activity, and losing excess weight can often slow or prevent the progression to type 2 diabetes. Regular check-ups with your healthcare provider and routine blood glucose testing are also important to manage this condition and monitor for the development of type 2 diabetes.
Can waist size be used to indicate risk of developing type 2 diabetes?
Waist size can be a significant indicator of the risk of developing type 2 diabetes. Excess abdominal fat, particularly visceral fat that surrounds organs in the abdominal cavity, is closely linked to insulin resistance and an increased risk of type 2 diabetes.
A large waist circumference is associated with a higher risk of developing type 2 diabetes, independent of overall body weight. The cutoff points for increased risk may vary depending on factors like ethnicity, but generally, the following guidelines are used:
- For men, a waist circumference of 40 inches (102 cm) or more is considered high risk
- For women, a waist circumference of 35 inches (88 cm) or more is considered high risk
However, it’s important to note that these values are not universally applicable and can vary based on factors such as height, body composition, and individual characteristics.
Measuring waist circumference is a simple procedure that can be done at home. To measure your waist:
- Stand up straight and breathe normally
- Locate the top of your hip bones
- Place a measuring tape around your waist at the level of your belly button
- Make sure the tape is snug but not too tight, and ensure it’s parallel to the floor
- Take the measurement at the end of a normal exhalation
Remember that waist circumference is just one aspect of assessing the risk of type 2 diabetes. Other factors such as family history, lifestyle, overall health, and blood tests are also important considerations. If you have concerns about your risk for diabetes, it’s advisable to consult with a healthcare professional who can provide a comprehensive evaluation and guide you on preventive measures and appropriate management.
What are the treatment and management options for type 2 diabetes?
The treatment and management of type 2 diabetes typically involve a combination of lifestyle modifications, medications, and regular monitoring. Here are some common approaches:
Lifestyle modifications
These play a crucial role in managing type 2 diabetes. They include:
- Healthy eating: Adopting a balanced diet that focuses on whole grains, lean proteins, fruits, vegetables, and healthy fats. Limiting the intake of sugary foods, processed foods, and unhealthy fats is important
- Regular physical activity: Engaging in regular exercise, such as brisk walking, cycling, or swimming, helps improve insulin sensitivity and blood sugar control. Strive for at least 150 minutes of moderate-intensity aerobic activity per week, along with strength training exercises
- Weight management: Achieving and maintaining a healthy weight through a combination of healthy eating and regular physical activity can significantly improve blood sugar control
Oral medications
Depending on your specific needs and the progression of the condition, your healthcare provider may prescribe oral medications to help lower blood sugar levels. These medications work in various ways, such as stimulating insulin production, improving insulin sensitivity, or reducing glucose production by the liver.
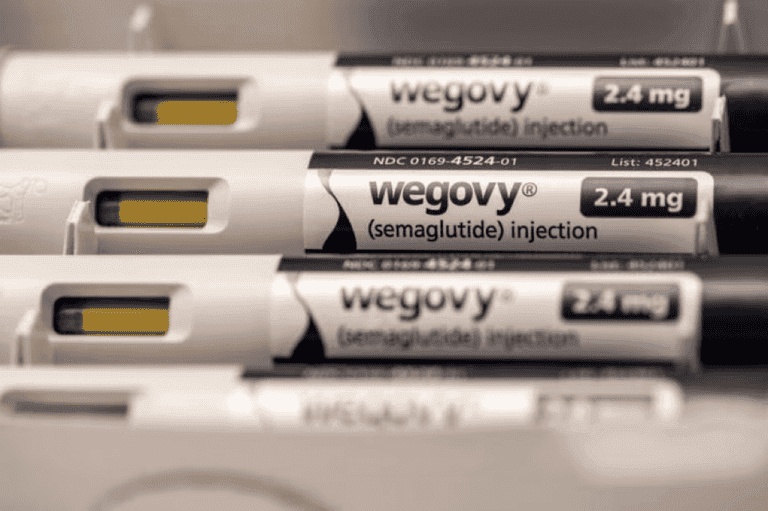
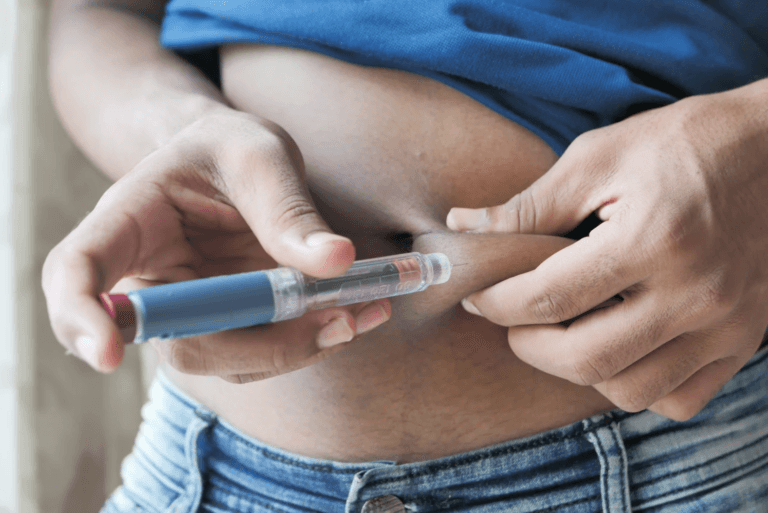
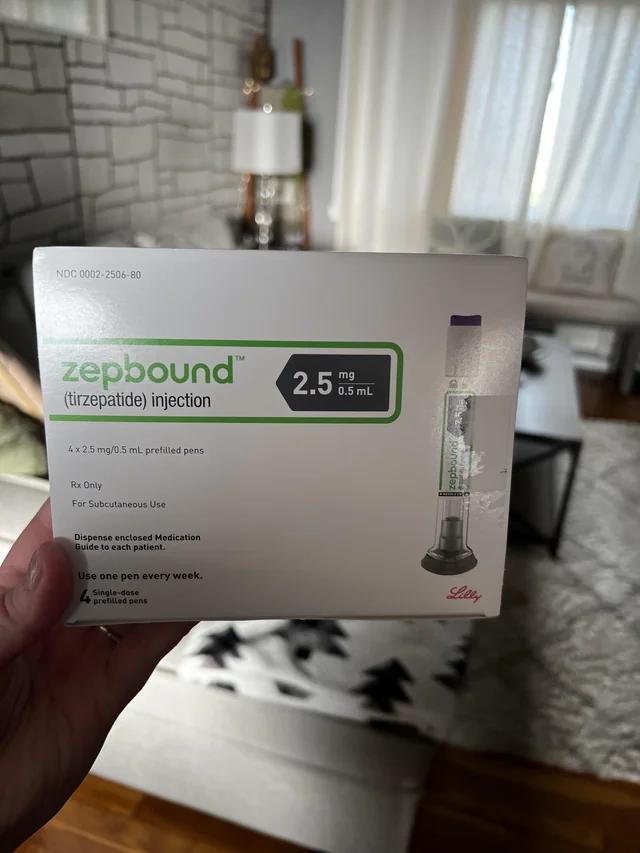
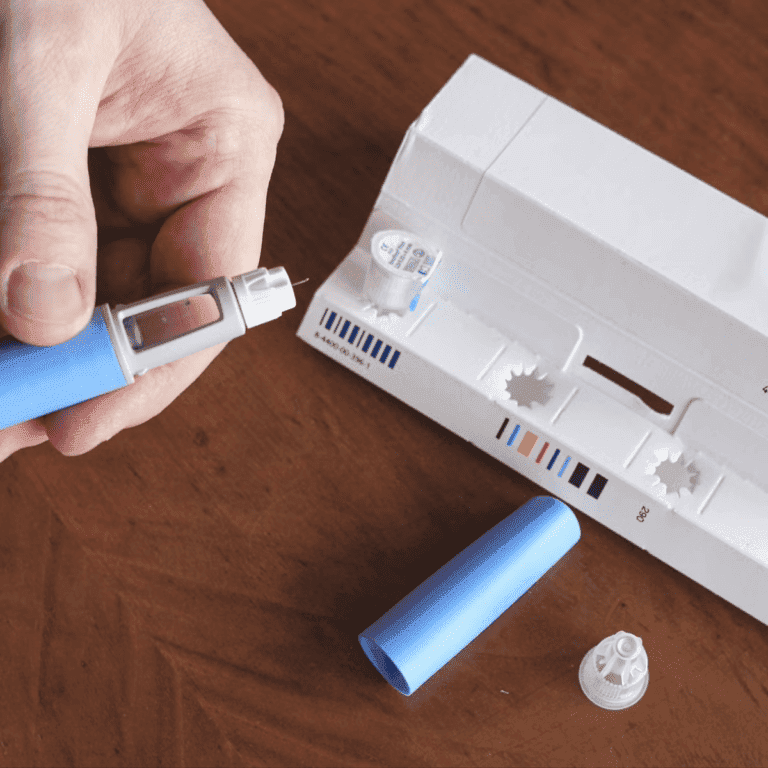
Injectable medications
In some cases, injectable medications such as GLP-1 receptor agonists or insulin therapy may be necessary to manage blood sugar levels effectively. These medications may be used alone or in combination with oral medications.
Blood sugar monitoring
Regular monitoring of blood sugar levels helps track how well your treatment plan is working and enables adjustments as needed. This can be done using a blood glucose meter or continuous glucose monitoring (CGM) devices.
Regular check-ups and screenings
Routine visits to your healthcare provider are important to monitor your overall health, review blood sugar control, assess any complications, and adjust your treatment plan if necessary. Additionally, screenings for other health parameters like blood pressure, cholesterol levels, kidney function, and eye examinations are usually recommended.
Diabetes education and support
Diabetes self-management education and support programs can provide valuable knowledge, skills, and emotional support to help you effectively manage your diabetes. These programs often cover topics like healthy eating, physical activity, medication management, blood sugar monitoring, and coping with the emotional aspects of living with diabetes.
Remember, the treatment and management plan for type 2 diabetes may vary for each individual. It’s essential to work closely with your healthcare team to develop a personalized approach that suits your specific needs, lifestyle, and health goals.
What medications are used in type 2 diabetes?
Metformin
Metformin is often the first-line medication for Type 2 Diabetes. It helps lower blood glucose levels by reducing glucose production in the liver and improving insulin sensitivity.
Sulfonylureas
- Glimepiride (Amaryl)
- Glipizide (Glucotrol)
- Glyburide (Diabeta, Micronase)
Meglitinides
- Repaglinide (Prandin)
- Nateglinide (Starlix)
Dipeptidyl Peptidase-4 (DPP-4) Inhibitors
- Sitagliptin (Januvia)
- Saxagliptin (Onglyza)
- Linagliptin (Tradjenta)
Sodium-Glucose Co-Transporter 2 (SGLT2) Inhibitors
- Canagliflozin (Invokana)
- Dapagliflozin (Farxiga)
- Empagliflozin (Jardiance)
Thiazolidinediones (TZDs)
- Pioglitazone (Actos)
- Rosiglitazone (Avandia)
Alpha-Glucosidase Inhibitors
- Acarbose (Precose)
- Miglitol (Glyset)
Glucagon-like Peptide-1 (GLP-1) Receptor Agonists
- Exenatide (Byetta, Bydureon)
- Liraglutide (Victoza, Saxenda)
- Dulaglutide (Trulicity)
- Semaglutide (Ozempic)
Basal Insulin Injections
- Insulin glargine (Lantus, Basaglar, Toujeo)
- Insulin detemir (Levemir)
Combination Medications
Combination medications may include a mix of two or more of the above classes, such as metformin combined with a sulfonylurea or a DPP-4 inhibitor.
Supplements
- chromium
- Biotin
- Carnitine (L-Carnitine, Acetyl L-Carnitine)
- Magnesium
What are the complications and prevention strategies for type 2 diabetes?
Type 2 diabetes, if not well managed, can lead to various complications affecting different parts of the body. However, many of these complications can be prevented or delayed through proper management and lifestyle interventions. Here are some common complications associated with type 2 diabetes and prevention strategies:
Cardiovascular disease
People with diabetes have an increased risk of heart disease, stroke, and other cardiovascular conditions. Prevention strategies include:
- Managing blood pressure and cholesterol levels within target ranges
- Adopting a heart-healthy diet, low in saturated and trans fats
- Engaging in regular physical activity
- Avoiding smoking and reducing alcohol consumption
Kidney disease (diabetic nephropathy)
High blood sugar levels and uncontrolled diabetes can damage the kidneys. Prevention strategies include:
- Maintaining good blood sugar control
- Managing blood pressure within target ranges
- Regularly monitoring kidney function through blood and urine tests
Eye complications (diabetic retinopathy)
Diabetes can lead to vision problems and even blindness. Prevention strategies include:
- Regular eye examinations by an ophthalmologist
- Good blood sugar and blood pressure control
- Avoiding smoking
Nerve damage (diabetic neuropathy)
Long-term uncontrolled diabetes can cause nerve damage, leading to pain, numbness, and loss of sensation in the extremities. Prevention strategies include:
- Maintaining good blood sugar control
- Regular foot care and daily inspection for any sores or injuries
- Managing blood pressure and cholesterol levels
Foot complications
Poorly managed diabetes can lead to foot ulcers, infections, and in severe cases, amputations. Prevention strategies include:
- Regular foot inspections and proper foot care
- Wearing comfortable, well-fitting shoes
- Promptly treating any foot injuries or infections
Other complications
Diabetes can also increase the risk of skin infections, dental problems, hearing impairment, depression, and cognitive decline. Prevention strategies include:
- Maintaining good overall health and well-being
- Regular medical and dental check-ups
- Seeking appropriate treatment and support for mental health
Prevention of complications primarily relies on effectively managing diabetes. This includes adhering to the prescribed treatment plan, maintaining healthy blood sugar levels, managing blood pressure and cholesterol, adopting a healthy lifestyle, and attending regular medical check-ups.
Can a type 2 diabetic have a hypoglycemia?
People with Type 2 Diabetes can experience hypoglycaemia. This happens when blood sugar levels drop too low. This can be easily remedied by ingesting the right carbohydrates. Severe hyproglycemia, however, is a medical emergency.
Although hypoglycemia is most common in people who are insulin dependent type 1 diabetics, there is a rise in prevalence of hypoglycemia in type 2 diabetics who are being treated with Insulin therapy or taking medication to reduce high blood sugar.
Triggers can include:
- undertaking sudden physical activity
- eating too little food
- drinking excessive alcohol
Symptoms of hyperglycaemia include:
- blurred vision
- tiredness
- increased thirst and a dry mouth
- needing to pee frequently
- rapid weight loss
- recurrent infections, such as thrush
Causes of hyperglycemia include:
- onset of illnesses like a common cold
- increased stress
- eating too much, such as snacking between meals
- dehydration
- missing a dose of prescribed medication for diabetes
- taking an incorrect dose of diabetic medication
- taking medications to treat other conditions such as steroid medications
Carbohydrate consumption and type 2 diabetes
Type 2 diabetes is a condition in which individuals can produce insulin, but their bodies cannot utilize it as effectively as those without the condition. This is known as insulin resistance. To compensate for this, the body increases insulin production to aid in the transportation of glucose from the blood to the cells.
Type 2 diabetics who consume a diet rich in glycemic carbohydrates increase their insulin resistance and their body struggles to produce sufficient insulin.
To manage and counter insulin resistance, one can primarily reduce the body’s insulin production needs. This can be achieved by lowering calorie intake, including carbohydrate consumption, and engaging in regular physical activity.
Additionally, some individuals may need to take diabetes medication to maintain healthy sugar levels.
It’s important to note that reliance on medication could lead to more extensive side effects. Therefore, it is crucial to make efforts in managing the condition through the primary method of lifestyle changes.
In the UK, although the NHS does not typically recommend a low carb diet for people with type 2 diabetes, many patients have chosen to adopt this approach independently.
What type 2 diabetes support organisations are there available to support me in the UK?
- Diabetes UK: Diabetes UK is the leading charity in the UK dedicated to supporting people with diabetes, including Type 2 Diabetes. They provide information, resources, educational materials, online community forums, local support groups, and a helpline for individuals with diabetes and their families
- X-PERT Health: X-PERT Health is an organization that offers structured education programs for people with Type 2 Diabetes. Their courses cover various aspects of diabetes self-management, including nutrition, physical activity, medication management, and psychological well-being
- Diabetes Research & Wellness Foundation (DRWF): The DRWF supports all forms of diabetes, including Type 2 Diabetes. They provide educational resources, information, support programs, and events to help individuals manage their condition effectively. They also fund research to improve diabetes care and outcomes
What type 2 diabetes support organisations are there available to support me in the US?
- American Diabetes Association (ADA): The ADA is a leading national organization dedicated to supporting individuals with diabetes, including Type 2 Diabetes. They provide educational resources, advocacy initiatives, support groups, community programs, and information on managing diabetes effectively
- Beyond Type 2: Beyond Type 2 is a non-profit organization focused on supporting and empowering individuals with Type 2 Diabetes. They offer resources, personal stories, educational content, community connections, and tools to help individuals navigate life with Type 2 Diabetes
- DiabetesSisters: DiabetesSisters is a community-based organization that provides support and resources specifically for women with diabetes, including Type 2 Diabetes. They offer online forums, local meetup groups, educational events, and resources focused on women’s health and diabetes management
- TCOYD (Taking Control of Your Diabetes): TCOYD is an organization that provides education and support for individuals with diabetes, including Type 2 Diabetes. They offer conferences, workshops, online resources, and an active online community to help individuals better understand and manage their condition
- JDRF (formerly Juvenile Diabetes Research Foundation): While JDRF’s primary focus is on Type 1 Diabetes, they also provide resources, support, and advocacy initiatives for individuals with Type 2 Diabetes. They offer educational materials, community events, and fundraising opportunities
Summary
Type 2 diabetes is a prevalent chronic condition that requires lifelong management. Understanding the causes, symptoms, treatment options, and diabetes prevention measures is essential for individuals with diabetes risk and those living with the condition. By adopting a healthy lifestyle, working closely with healthcare professionals, and following prescribed treatments, individuals with type 2 diabetes can effectively manage their blood sugar levels, minimize complications, and lead a fulfilling life. Early detection, intervention, and ongoing self-care play pivotal roles in achieving optimal health outcomes for those affected by type 2 diabetes.
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.






















































































![An injection syringe on a white background. [Injection Semaglutide]](/_next/image?url=https%3A%2F%2Fnpcms.nowpatient.com%2Fwp-content%2Fuploads%2F2023%2F09%2FOral-Semaglutide-Vs.-Injection-Semaglutide-768x512.webp&w=3840&q=75)