Insulin is one of the most commonly prescribed medications for people with diabetes and it is essential for the proper regulation of blood sugar. However, like all medications, insulin can have side effects that need to be monitored. It’s important to understand these side effects so you can work with your doctor to manage them and maximise the benefits of insulin treatment.
Who needs to take insulin?
Diabetics
Insulin is most commonly prescribed to people with diabetes to help regulate blood sugar and prevent diabetic ketoacidosis. It can be used as part of a comprehensive diabetes management plan. Diabetes is a chronic medical condition, there are multiple types that can affect the body. The two main types of diabetes are Type 1 and Type 2 diabetes.
Type 1 diabetes, also known as diabetes mellitus, is caused by an autoimmune condition where the body’s own antibodies attach to cells in the pancreas, thus damaging them and causing insulin production to be stopped or greatly reduced. Insulin-dependent diabetes is another term that may sometimes be used to describe type 1 diabetes.
Type 2 diabetes usually results from insulin resistance (not enough insulin being produced from cells) combined with certain risk factors such as obesity, physical inactivity, unhealthy diet and high cholesterol. In addition, HbA1c levels might also be elevated which typically indicates high levels of sugar in the blood over a period of time. People with type 2 diabetes often need to take supplemental insulin as well as oral medications or lifestyle changes in order to control their blood sugar levels.
Prediabetes occurs when HbA1c values are slightly raised but not at a level which would mark it as type 2 diabetes yet.
Other Conditions
Insulin therapy isn’t just used for diabetes; it can also treat other conditions in which the body does not produce enough insulin. For example, some people with pancreatic cancer or cystic fibrosis may need to take supplemental doses of insulin if their bodies cannot produce enough on their own. In addition, women with polycystic ovarian syndrome (PCOS) can benefit from taking small doses of insulin if they have difficulty controlling their blood sugar levels due to the condition.
How is insulin taken?
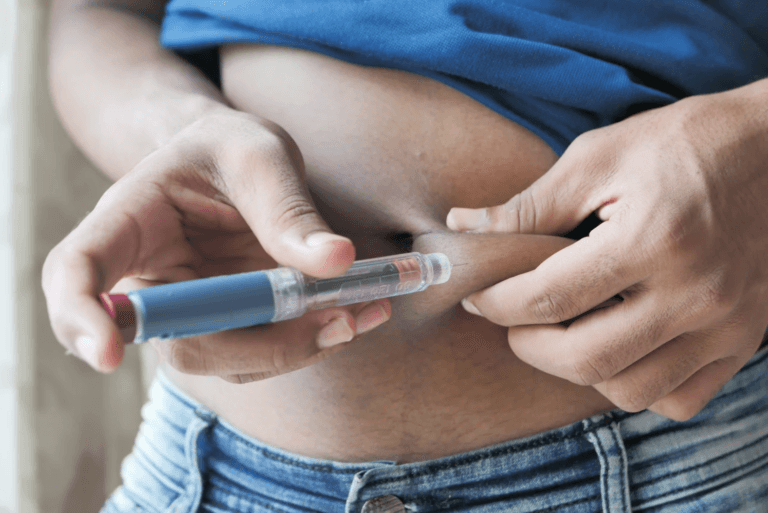
Taking insulin is an important part of managing diabetes and can help you keep your blood sugar under control. There are several different ways to take insulin and it is important to discuss them with a doctor or pharmacist in order to find the best option for you. Insulin is usually taken via injection, but now there are also insulin pens, pumps and inhalable spray forms. Injection therapies consist of needle injections or jet injectors, which don’t use needles. Insulin pens allow for pre-filled cartridges that are easy to use. For the insulin pump, a device is worn on your body which releases a steady stream of insulin throughout the day into your skin. Finally, with inhalable forms of insulin, an individual would inhale a powdered form through their mouth or nose. Talk to your healthcare provider today regarding which form of taking insulin would be best for you!
Types of insulin
There are several types of insulin used to treat diabetes and understanding the differences can be quite daunting. In simple terms: Short-acting insulins work very quickly but have a short-term duration of effect – usually no longer than five hours. Long-acting insulins, such as glargine, provide you with a steady amount of insulin all day long. Some people may find that they need extra short-acting insulin before meals to help with blood glucose control.
How does insulin work?
Insulin helps your body move glucose from your bloodstream into your cells so that it can be used for energy. When you eat foods that contain carbohydrates (like bread, pasta, fruits and vegetables), your blood sugar levels rise due to the release of glucose into your bloodstream. The pancreas secretes insulin into the bloodstream in response to this rise in blood sugar levels so that the glucose can be moved into your cells where it can be used for energy. Without enough insulin, cells cannot absorb enough sugar, resulting in high blood sugar levels within the bloodstream (hyperglycemia). This can have serious health consequences over time such as the increased risk of high blood pressure, heart disease, blurred vision and organ damage.
Side effects of insulin
While insulin is generally very safe when taken as prescribed, there are potential side effects associated with it.
Hypoglycemia
One of insulin’s most common side effects is hypoglycemia or low blood sugar. People with diabetes often experience hypoglycemia when their blood glucose levels drop too low due to taking too much insulin or missing a meal. Symptoms of hypoglycemia include dizziness, sweating, confusion and dizziness. If you experience any of these symptoms after taking insulin, it’s important to test your blood sugar levels and eat something sweet like candy or juice to raise your glucose levels back up.
Weight Gain
Weight gain can be a surprising and unwanted side effect of taking insulin, but understanding why it occurs can provide insight into how to avoid it. Insulin makes cells in the body absorb glucose as fuel and store it as fat, causing people to gain weight. Additionally, when blood sugar levels are controlled with insulin, people often experience an increase in appetite, which might lead them to eat more than they normally would. Although changing your diet is important, some added weight while managing diabetes is common and should not be a cause for concern. However, it is possible to combat this side effect by being mindful of a balanced diet full of nutrient-rich foods and maintaining regular physical activity if able. Patients should be sure to check in with their healthcare provider as they manage their diabetes, as they can provide tips on ways to combat any weight gain related to insulin usage.
Allergic Reactions
In rare cases, people may experience allergic reactions when taking insulin such as rashes or hives on the skin or swelling in the face or throat area. If you experience symptoms like these after taking insulin, stop taking it immediately and seek medical help immediately. It could be dangerous if left untreated so take action quickly if you suspect an allergic reaction has occurred.
Injection site reactions
One of the most common side effects of using insulin is injection site reactions, such as redness and/or irritation at the injection sites. These types of skin reactions occur when your body is responding to what it perceives as an intruder, similar to an allergic reaction. Unfortunately, skin responses like this are quite common and happen to even the most experienced insulin users. The best thing you can do if you experience any sort of reaction at or near your injection site is to take a break from injecting in that area and rotate to other injection sites on your body instead. If you are having frequent reactions or they seem overly strong, it may be a good idea to consult with your healthcare provider to ensure that your insulin dosage or delivery method is appropriate for you.
Skin changes at the injection site (lipodystrophy)
Insulin injection therapy involves taking injections of insulin for people with diabetes. This is done to help regulate blood sugar and can be used as part of a comprehensive diabetes management plan. An injection typically only takes a few seconds, most patients find the entire procedure entirely painless.
Lipodystrophy, or changes to the skin at the injection site of insulin therapy, is a common side effect of taking insulin. It can present as lumps or lipohypertrophy (thickened flesh) and can be anywhere the insulin is injected. Lipoatrophy (depressed areas) may also occur due to fat loss. Fortunately, these conditions are generally only cosmetic and do not affect how well insulin works. As such, regularly changing the injection sites is often recommended, to avoid developing lipodystrophic conditions. It’s also important to make sure your hands are clean before each injection and to always inject at room temperature. Consult your healthcare professional if you want to know more about avoiding adverse outcomes associated with insulin therapy.
Swelling of your arms and legs
Swelling of your arms and legs due to insulin therapy is a common side effect, but it can be worrisome. The most likely explanation for this is that the rise in insulin levels causes extra fluid to be pulled into the arm or leg tissues. The good news is that this type of swelling is usually harmless and can easily be relieved with simple steps, like avoiding standing or sitting in one position for too long and elevating your legs when you rest. If you find yourself experiencing this side effect, speak to your healthcare provider immediately – they will help determine the cause and provide specific advice on how to reduce swelling.
Low potassium
Low blood potassium, also known as hypokalemia, is a common side effect of taking insulin. While it may cause some discomfort such as weak muscles, cramping, and fatigue, it is easy to manage. The most effective way to lower the risks of hypokalemia is to eat foods that are rich in potassium such as bananas and oranges. Drinking plenty of fluids can also help because they increase the level of potassium in the body by making it easier for the kidneys to absorb it and normalise levels. Additionally, your physician may suggest regular glucose testing and monitoring of your blood pressure, in order to identify any changes related to your insulin dosage. Despite its unpleasant symptoms, if hypokalemia is properly managed with a combination of diet and medication prescribed by your doctor, you’ll be able to enjoy a healthy lifestyle with peace of mind.
Drug interactions
When taking insulin, it is important to be aware of potential drug interactions that can increase your risk for serious side effects. The result of these interactions can be dangerous and even life-threatening. Some medications that commonly interact with insulin and may increase blood sugar levels are:
- Steroids
- Isoniazid
- Oral contraceptives
- Thyroid drugs
- Thiazides
Other drugs that may require a person to use less insulin are:
- Aspirin
- Monoamine oxidase inhibitors
- Angiotensin-converting enzyme inhibitors
- Beta-blockers
- Oral diabetes medications e.g. rosiglitazone
It is essential to inform your doctor of any prescription or over-the-counter medications, vitamins, herbs and supplements you are currently taking, so they may determine if any changes are necessary for the course of your treatment with insulin. In addition, always read the warnings on the label when taking new medicines and ask a pharmacist if you have any questions about possible interactions before starting any new drugs. By being informed and vigilant, you may significantly reduce the risk of serious side effects associated with insulin use.
Insulin has been proven as an effective treatment for diabetes but like all medications, there are risks associated with its use, including hypoglycemia, weight gain and allergic reactions. With proper monitoring and care from a healthcare team experienced in treating diabetes, these risks can be minimised while still providing effective treatment for diabetes-related symptoms. If you have any concerning symptoms while on insulin therapy, it’s important to discuss them with your healthcare provider right away, in order to ensure your safety and wellness during treatment.
Sources
- Human Insulin Injection – Medline Plus
- Understanding medicine -Type 2 diabetes – NHS
- WELCOME TO THE GLOBAL DIABETES COMMUNITY – Diabetes
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.