Type 1 Diabetes
Get valuable insights into Type 1 Diabetes, including its causes, symptoms, prevention strategies, and treatment options, while also learning about how you can lower the cost of the medications used to treat Type 1 Diabetes.
MEDICAL INFORMATION
Type 1 Diabetes Key Facts
Related Medications
What is the definition of type 1 diabetes?
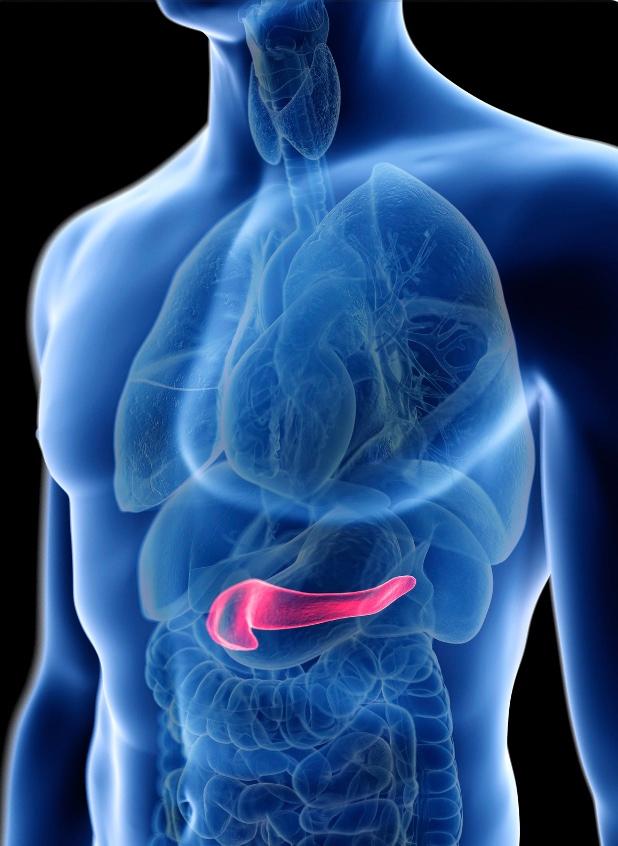
Type 1 diabetes is characterized by the destruction of insulin-producing pancreatic beta cells in the pancreas by the immune system T cells, resulting in not enough insulin production. Insulin is a hormone necessary for regulating blood sugar levels and allowing glucose to enter cells for energy.
What are the causes and risk factors associated with type 1 diabetes?
Type 1 diabetes is an autoimmune condition where the immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. The exact cause of type 1 diabetes is not fully understood, but it is believed to involve a combination of genetic and environmental factors. Here are some of the known causes and risk factors associated with type 1 diabetes:
- Genetics: Certain genes contribute to the susceptibility of developing type 1 diabetes. Having specific human leukocyte antigen (HLA) genes, such as HLA-DR3, HLA-DR4, or HLA-DQ8, increases the risk. However, not everyone with these genes develops type 1 diabetes, indicating that other factors are involved
- Autoimmune factors: Type 1 diabetes is considered an autoimmune disease, where the immune system mistakenly attacks the insulin-producing cells in the pancreas. The exact triggers that initiate this autoimmune response are still under investigation
- Environmental factors: Environmental factors, such as viral infections, toxins, or dietary factors, may play a role in triggering the autoimmune response in genetically susceptible individuals. However, the specific environmental triggers have not been definitively identified
- Family history: Having a close family member, such as a parent or sibling, with type 1 diabetes increases the risk. However, most people with a family history of type 1 diabetes do not develop the condition
- Age: Although type 1 diabetes can occur at any age, it is more commonly diagnosed in children, adolescents, and young adults. The peak age of onset is around puberty
- Race and ethnicity: Type 1 diabetes is more prevalent in certain racial and ethnic groups, including people of Northern European, Caucasian, and Scandinavian descent. However, it can occur in individuals of any race or ethnicity
It’s important to note that the causes and risk factors mentioned above relate specifically to type 1 diabetes. Type 2 diabetes, on the other hand, has distinct causes and risk factors. Understanding these differences is essential for accurate diagnosis, appropriate management, and tailored care for individuals with diabetes.
What are the symptoms of type 1 diabetes?
Type 1 diabetes often develops rapidly, and the diabetes symptoms can appear suddenly. It’s important to be aware of these symptoms and seek medical attention if you experience them. The common symptoms of type 1 diabetes include:
- Excessive thirst: Feeling extremely thirsty and having an unquenchable desire to drink fluids
- Frequent urination: Increased need to urinate, including waking up multiple times during the night to urinate (nocturia)
- Unexplained weight loss: Despite eating normally or even more than usual, rapid and unexplained weight loss can occur
- Increased hunger: Persistent feelings of hunger, even shortly after eating a meal
- Fatigue and weakness: Feeling unusually tired and lacking energy, even with sufficient rest
- Blurred vision: Vision may become blurry or distorted
- Frequent infections: Increased susceptibility to infections, such as urinary tract infections (UTIs), yeast infections, or skin infections
- Slow healing of wounds: Cuts, sores, or wounds may take longer to heal than usual
- Irritability and mood changes: Sudden mood swings, irritability, or unexplained changes in behaviour
- Fruity-smelling breath: Breath may have a sweet or fruity odour due to the presence of ketones in the body
It’s important to note that these symptoms may not be exclusive to type 1 diabetes and can also be associated with other health conditions. If you experience any of these symptoms or suspect you may have diabetes, it’s crucial to seek medical evaluation and get a proper diagnosis. Early detection and prompt management are vital in type 1 diabetes to prevent complications and maintain optimal health.
How is type 1 diabetes diagnosed?
The diagnosis of type 1 diabetes involves a combination of clinical symptoms, blood tests, and medical evaluations. Below is an overview of the typical diagnostic methods
Medical history and symptoms:
Your healthcare provider will inquire about your medical history, including any symptoms you have been experiencing. Symptoms such as excessive thirst, frequent urination, unexplained weight loss, increased hunger, and fatigue may raise suspicion of type 1 diabetes
Blood tests
Blood tests are essential for diagnosing diabetes. The following tests are commonly performed:
- Fasting plasma glucose (FPG) test: This test measures your blood sugar level after an overnight fast. A fasting plasma glucose level of 126 milligrams per deciliter (mg/dL) (UK equivalent of 7 mmol/L or over) higher on two separate occasions typically indicates diabetes
- Hemoglobin A1c (HbA1c) test: This test provides an average blood sugar level over the past two to three months. An HbA1c level of 6.5% or higher usually indicates diabetes. However, it’s important to note that HbA1c may not be as reliable in diagnosing type 1 diabetes in children or individuals with certain conditions
- Random blood sugar test: If you have severe symptoms of diabetes, such as extreme thirst, frequent urination, or fatigue, a random blood sugar test may be performed. A result of 200 mg/dL (11.1 mmol/L) or higher, along with symptoms, suggests diabetes
Autoantibody tests
Type 1 diabetes is an autoimmune condition, and autoantibodies specific to the disease are often present. Testing for the presence of autoantibodies, such as glutamic acid decarboxylase antibodies (GAD antibodies) or islet cell antibodies (ICA), can help confirm the diagnosis of type 1 diabetes
C-peptide test
C-peptide is a byproduct of insulin production. A low level of C-peptide in the blood may indicate a decreased production of insulin, supporting the diagnosis of type 1 diabetes
Additional tests
Depending on the situation, your doctor may order additional tests to evaluate your overall health, check for potential complications, and assess the function of various organs
It’s important to note that the specific diagnostic process may vary based on individual circumstances and healthcare practices. If you receive a diagnosis of type 1 diabetes, your healthcare provider will guide you further in terms of treatment, education, and ongoing management. Regular follow-ups and maintaining good communication with your healthcare team are crucial for effectively managing type 1 diabetes and maintaining optimal health.
What are the treatment and management options for type 1 diabetes?
The treatment and management of type 1 diabetes focus on maintaining healthy blood sugar levels, preventing complications, and promoting overall well-being. Here are the primary treatment and management options for type 1 diabetes:
- Insulin therapy: People with type 1 diabetes require insulin replacement since their pancreas does not produce insulin. Insulin is administered through injections or an insulin pump. Different types of insulin are available, including rapid-acting, short-acting, intermediate-acting, and long-acting insulin. The specific insulin regimen is tailored to individual needs and may involve multiple daily injections or continuous subcutaneous insulin infusion (CSII) via a pump
- Blood sugar monitoring: Regular self-monitoring of blood glucose levels is crucial for managing type 1 diabetes. This involves using a blood glucose meter to check blood sugar levels throughout the day. Frequent monitoring helps determine insulin doses, identify patterns, and make adjustments to maintain optimal blood sugar control
- Carbohydrate counting and meal planning: Understanding the impact of carbohydrates on blood sugar levels and following a consistent meal plan is important. Carbohydrate counting helps determine the appropriate insulin dose to match the food intake. Working with a registered dietitian or diabetes educator can provide guidance on meal planning, portion sizes, and balancing nutrition
- Physical activity: Regular physical activity is beneficial for managing blood sugar levels, improving insulin sensitivity, and promoting overall health. It’s important to work with your healthcare team to develop an exercise plan that aligns with your diabetes management. Monitoring blood sugar levels before, during, and after exercise is essential to prevent hypoglycemia (low blood sugar) or hyperglycemia (high blood sugar)
- Education and support: Diabetes self-management education is crucial for understanding the condition, treatment strategies, and lifestyle modifications. It helps individuals develop skills for managing diabetes effectively, including blood sugar monitoring, insulin administration, healthy eating, and problem-solving. Support from healthcare providers, diabetes educators, support groups, and online communities can provide valuable guidance and emotional support
- Regular check-ups and screenings: Ongoing medical care, including regular check-ups, is essential for monitoring blood sugar control, assessing overall health, and identifying and managing any potential complications. Screening for complications such as eye exams, kidney function tests, cholesterol checks, and foot examinations are typically recommended
Remember, each person with type 1 diabetes has unique needs, and treatment plans should be individualized. Working closely with a healthcare team, including endocrinologists, diabetes educators, dietitians, and other specialists, helps tailor the treatment approach, address specific concerns, and promote long-term health and well-being.
What is a CGM and how does it help type 1 diabetics?
Continuous Glucose Monitoring (CGM) is an advanced technology used in the management of type 1 diabetes. It provides continuous real-time measurements of glucose levels throughout the day and night, offering valuable insights into blood sugar trends and patterns. Here are some key points about CGM in type 1 diabetics:
How it works
CGM systems consist of a small sensor inserted under the skin, usually on the abdomen or arm, which measures glucose levels in the interstitial fluid. The sensor is connected to a transmitter that wirelessly sends the glucose data to a receiver or a compatible smart device. Users can view their glucose readings and trends in real-time, helping them make more informed decisions about their diabetes management
Benefits of CGM
CGM offers several advantages for people with type 1 diabetes, including:
- Real-time monitoring: CGM provides continuous glucose readings, helping users detect high or low blood sugar levels promptly and take appropriate action
- Trend analysis: CGM displays glucose trends, showing the direction and rate at which blood sugar levels are changing. This information can help individuals make adjustments to their insulin doses, diet, and physical activity
- Alerts and alarms: CGM systems can be programmed to alert users when their glucose levels are too high or too low. This can be especially helpful during sleep or other times when the user may not be actively monitoring their glucose levels
- Insulin dosing assistance: Some CGM systems integrate with insulin pumps or insulin management apps, providing guidance on insulin dosing decisions based on current glucose levels and trends
Data analysis and pattern recognition
CGM systems often include software or mobile apps that allow users to review their glucose data over specific time periods. Users and their healthcare providers can analyze the data, identify patterns, and make informed adjustments to their diabetes management plan
Accuracy and calibration
CGM systems have improved in accuracy over the years, but occasional calibration may still be required. Calibration involves comparing CGM readings with blood glucose meter readings and adjusting the CGM system as needed to ensure accurate measurements
Integration with insulin pumps
Some CGM systems can communicate directly with insulin pumps, enabling automatic adjustments to insulin delivery based on glucose readings. This feature, known as sensor-augmented pump therapy or hybrid closed-loop systems, helps optimize blood sugar control
Accessibility
CGM systems may be covered by insurance in the US, but coverage policies can vary. It’s important to check with your insurance provider to understand the specific coverage and requirements. Additionally, advancements in technology have made CGM more accessible and user-friendly over time. In the UK, the NHS provides CGM to most Type 1 diabetics
Newer diabetes technology
Apps like Quintech aim to assist individuals in managing their diabetes by providing tools for tracking blood sugar levels, medication, meals, physical activity, and other relevant data. Users connect their CGM to the app, and then input data like insulin dosing, foods eaten, exercise undertaken etc. After 10 days of data collection, Quin Diabetes App, using AI and ML, can present the user with a personalised ‘what’s ahead’ graph, showing the effect their proposed actions or decisions on their blood sugar. This can considerably improve the Type 1 Diabetic’s quality of life
Can type 1 diabetes be cured?
Currently, there is no known cure for type 1 diabetes. Type 1 diabetes is an autoimmune condition where the insulin-producing cells in the pancreas are destroyed, resulting in a lifelong dependence on insulin therapy. However, with proper management and treatment, individuals with type 1 diabetes can lead healthy and fulfilling lives.
The primary goal of treatment for type 1 diabetes is to maintain normal blood sugar levels and prevent complications. This typically involves insulin replacement therapy, regular blood sugar monitoring, adherence to a healthy diet, physical activity, and ongoing education and support.
While there is ongoing research into potential cures for type 1 diabetes, such as islet cell transplantation and immunotherapy approaches, these treatments are still in the experimental stage and not widely available. The focus of current treatments is to effectively manage the condition, minimize the risk of complications, and enhance quality of life.
What medications are used in type 1 diabetes?
Insulin Injections
- Rapid-acting insulin analogs: Examples include insulin lispro (Humalog), insulin aspart (Fiasp, Novorapid), and insulin glulisine (Apidra)
- Short-acting insulin: Regular human insulin (Humulin R, Novolin R) falls into this category
- Intermediate-acting insulin: NPH insulin (Humulin N, Novolin N) is an example
- Long-acting insulin analogs: Examples include insulin glargine (Lantus, Basaglar, Toujeo), insulin detemir (Levemir), and insulin degludec (Tresiba)
Insulin Pump Therapy
- Insulin pumps deliver a continuous supply of rapid-acting insulin throughout the day and allow for precise dosage adjustments
Glucagon
- Glucagon emergency kit: Glucagon is used to treat severe hypoglycemia when a person with Type 1 Diabetes is unable to consume food or drink
What are the complications and prevention techniques for type 1 diabetes?
Type 1 diabetes can lead to various complications if blood sugar levels are not properly managed over time. Here are some of the potential complications associated with type 1 diabetes:
Hypoglycemia
Low blood sugar levels can occur if insulin or other diabetes medications are taken in excess, or if meals and snacks are not consumed on time. Hypoglycemia can cause symptoms like shakiness, dizziness, sweating, confusion, and, if severe, can lead to unconsciousness or seizures
Hyperglycemia and Diabetic Ketoacidosis (DKA)
High blood sugar levels, if not addressed, can lead to a condition called diabetic ketoacidosis. DKA is a medical emergency that can cause symptoms like excessive thirst, frequent urination, nausea, vomiting, abdominal pain, fruity-smelling breath, and confusion
Long-term complications
Poorly controlled blood sugar levels over time can increase the risk of long-term complications affecting various parts of the body, including:
- Cardiovascular complications: Type 1 diabetes increases the risk of heart disease, heart attacks, stroke, and narrowing of blood vessels (atherosclerosis)
- Kidney damage (diabetic nephropathy): Persistent high blood sugar levels can damage the kidneys and impair their function, potentially leading to chronic kidney disease or kidney failure
- Eye damage (diabetic retinopathy): Diabetes can affect the blood vessels in the retina, leading to vision problems, including blindness if left untreated
- Nerve damage (diabetic neuropathy): High blood sugar levels can damage the nerves, resulting in symptoms such as numbness, tingling, pain, and weakness, commonly affecting the feet and hands
- Foot complications: Diabetes-related nerve damage and poor blood circulation can lead to foot ulcers, infections, and, in severe cases, amputation
- Skin conditions: Diabetes can increase the risk of skin conditions, including bacterial and fungal infections, as well as slow wound healing
Prevention techniques for type 1 diabetes complications involve
- Maintaining target blood sugar levels: Regular monitoring of blood sugar levels and making necessary adjustments in insulin doses, diet, and physical activity to keep blood sugar levels within the target range
- Adopting a healthy lifestyle: Eating a balanced diet, engaging in regular physical activity, maintaining a healthy weight, avoiding tobacco use, and managing stress levels can contribute to overall well-being and minimize the risk of complications
- Regular medical check-ups: Regular visits to healthcare providers for comprehensive diabetes care, including monitoring of blood pressure, cholesterol levels, kidney function, eye health, and foot examinations
- Education and self-management: Being knowledgeable about diabetes management, understanding medications and their proper usage, and actively participating in self-care can help prevent complications. Diabetes education programs and support from healthcare professionals can provide valuable guidance and support in managing the condition effectively
What type 1 diabetes support organisations are there available to support me in the UK?
- JDRF (Juvenile Diabetes Research Foundation): JDRF is a leading charity dedicated to funding research and providing support for people with Type 1 Diabetes. They offer information resources, community support, advocacy, and fundraising opportunities
- Diabetes UK: Although Diabetes UK supports all types of diabetes, they provide resources and support for people living with Type 1 Diabetes as well. They offer information, educational resources, a helpline, local support groups, and an online community
- INPUT Diabetes: INPUT Diabetes is a charity that focuses on providing support, education, and advocacy for people with diabetes who use insulin pumps or continuous glucose monitoring (CGM) systems. They offer resources, training, and advice to help individuals make informed decisions about their diabetes management
- DRWF (Diabetes Research & Wellness Foundation): The DRWF supports all forms of diabetes, including Type 1 Diabetes. They provide educational resources, information, and support to help individuals manage their condition effectively. They also fund research and organize events to raise awareness
What type 1 diabetes support organisations are there available to support me in the US?
- JDRF (formerly Juvenile Diabetes Research Foundation): JDRF is a leading global organization dedicated to funding research and advocating for Type 1 Diabetes. They offer support programs, community events, information resources, advocacy initiatives, and fundraising opportunities
- Beyond Type 1: Beyond Type 1 is a non-profit organization that aims to improve the lives of those living with Type 1 Diabetes. They provide support through online resources, community connections, programs for children and families, educational content, and advocacy efforts
- American Diabetes Association (ADA): The ADA is a national organization that supports all types of diabetes, including Type 1 Diabetes. They offer educational materials, advocacy initiatives, support groups, community programs, and resources for managing diabetes effectively
- T1D Exchange: T1D Exchange is a non-profit organization that focuses on accelerating research, innovation, and access to therapies for people with Type 1 Diabetes. They provide support, resources, and opportunities for participation in research studies and clinical trials
- College Diabetes Network (CDN): CDN is an organization that supports young adults with Type 1 Diabetes who are transitioning to college and university life. They provide resources, support networks, and educational programs to help students manage their diabetes while pursuing higher education
- DiabetesSisters: Although DiabetesSisters primarily focuses on women with diabetes, they provide support and resources for women living with Type 1 Diabetes as well. They offer online forums, local meetup groups, educational events, and resources specific to women’s health and diabetes management
Summary
Type 1 diabetes is a lifelong condition that requires careful management and monitoring of blood sugar levels. Understanding the causes, recognizing the symptoms, and seeking early medical intervention are crucial for effective treatment and minimizing the risk of complications.
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.