Coronary Heart Disease
Get valuable insights into Coronary Heart Disease, including its causes, symptoms, prevention strategies, and treatment options, while also learning about how you can lower the cost of the medications used to treat Coronary Heart Disease.
MEDICAL INFORMATION
Coronary Heart Disease Key Facts
Related Medications
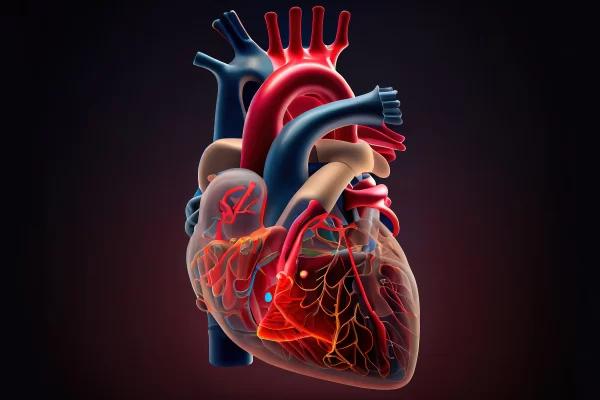
Coronary heart disease (CHD) is a prevalent and potentially life-threatening condition that affects millions of people worldwide. It is the leading cause of death globally, characterized by the narrowing or blockage of the coronary arteries, which supply oxygen-rich blood to the heart muscle. Here we aim to provide you with a detailed overview of coronary heart disease by exploring its definition, risk factors, pathophysiology, clinical manifestations, diagnosis, treatment options, and prevention strategies. Additionally, we will highlight recent advancements and emerging research in the field.
What is the definition of coronary heart disease?
Coronary heart disease (CHD), also known as coronary artery disease (CAD), is a cardiovascular condition characterized by the narrowing or blockage of the coronary arteries that supply blood to the heart muscle. It is a result of atherosclerosis, a condition where fatty deposits called plaques accumulate in the inner walls of the coronary arteries, leading to the narrowing of the arterial lumen. Over time, these plaques can become unstable, rupture, and form blood clots that further obstruct blood flow to the heart.
The reduced blood flow and oxygen supply to the heart muscle can result in various clinical manifestations, ranging from stable angina (chest pain or discomfort with physical exertion or stress) to acute coronary syndrome (ACS), including unstable angina and myocardial infarction (heart attack).
Coronary heart disease is a chronic and progressive condition that can lead to significant complications such as heart failure, arrhythmias, and even sudden cardiac death. It is a major global health concern, accounting for a substantial number of deaths worldwide. Early diagnosis, appropriate management, and lifestyle modifications are crucial in preventing disease progression and improving outcomes for individuals with coronary heart disease.
What is the pathophysiology of coronary heart disease?
The pathophysiology of coronary heart disease (CHD) involves a complex interplay of various factors, primarily driven by atherosclerosis. Atherosclerosis is a chronic inflammatory process characterized by the buildup of fatty plaques within the walls of the coronary arteries. Below are the pathophysiological mechanisms involved in the development and progression of CHD:
Endothelial dysfunction
The process of atherosclerosis begins with endothelial dysfunction, which is characterized by an impaired function of the endothelial cells lining the coronary arteries. This dysfunction is primarily caused by risk factors such as hypertension, smoking, diabetes, and high cholesterol levels. Endothelial dysfunction leads to increased permeability, recruitment of inflammatory cells, and the release of pro-inflammatory molecules.
Formation of fatty plaques
Under normal conditions, the endothelium acts as a protective barrier preventing the entry of lipids and immune cells into the arterial wall. However, in the presence of endothelial dysfunction, low-density lipoprotein (LDL) particles, particularly oxidized LDL, penetrate the endothelium and accumulate within the subendothelial space. Macrophages in the arterial wall engulf these lipids, transforming into foam cells and forming fatty streaks.
Inflammation and cellular response
The accumulation of LDL particles triggers an inflammatory response within the arterial wall. Inflammatory cells, such as monocytes and T lymphocytes migrate to the site of plaque formation. These immune cells release cytokines, growth factors, and enzymes that further promote inflammation and contribute to the progression of atherosclerosis.
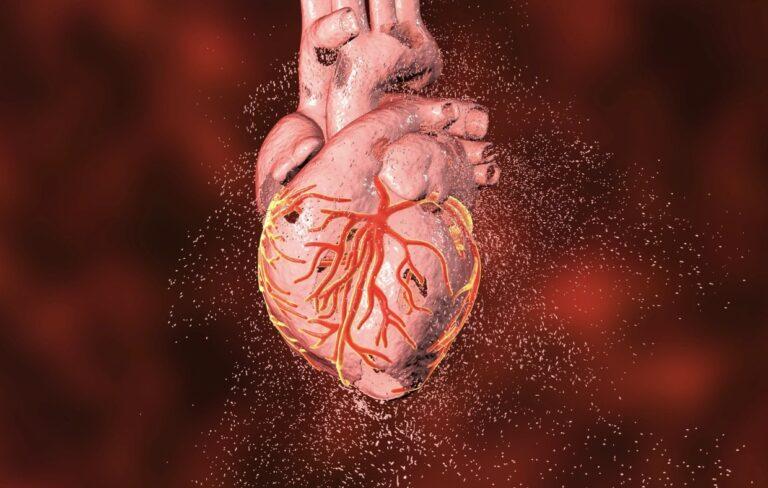
Plaque growth and complications
Over time, the fatty streaks within the arterial wall undergo further changes. Smooth muscle cells migrate to the site and proliferate, leading to the formation of a fibrous cap over the fatty plaque. This fibrous cap can become thick and unstable. Vulnerable plaques are characterized by a thin fibrous cap, a large lipid core, and a high degree of inflammation. These plaques are prone to rupture, leading to the formation of blood clots or thrombi.
Thrombosis and ischemia
Plaque rupture exposes the underlying thrombogenic material, including tissue factor and collagen, leading to platelet activation and aggregation. Platelets adhere to the site of plaque rupture, forming a thrombus that can partially or completely obstruct the coronary artery. The thrombus formation leads to acute coronary syndromes, such as unstable angina or myocardial infarction, resulting in reduced blood flow and oxygen supply to the heart muscle.
Collateral circulation
In some cases, chronic narrowing of the coronary arteries stimulates the growth of collateral blood vessels that provide an alternative route for blood flow to the ischemic heart muscle. Collateral circulation can partially compensate for the reduced blood flow and mitigate the symptoms of ischemia.
It is important to note that the pathophysiology of CHD is influenced by various risk factors, including hypertension, dyslipidemia, diabetes, smoking, and genetic predisposition. These risk factors can exacerbate endothelial dysfunction, inflammation, and plaque formation, accelerating the progression of atherosclerosis and increasing the likelihood of complications associated with CHD.
Understanding the pathophysiology of CHD helps in developing targeted prevention strategies, identifying potential therapeutic targets, and advancing diagnostic and treatment approaches for this prevalent cardiovascular condition.
What are the risk factors for coronary Heart disease?
Coronary heart disease (CHD) is influenced by a wide range of risk factors, both modifiable and non-modifiable. Identifying these risk factors is crucial in assessing an individual’s likelihood of developing CHD and implementing preventive measures. Let’s explore the various risk factors associated with CHD:
Modifiable risk factors
- Hypertension: High blood pressure puts additional strain on the coronary arteries, increasing the risk of atherosclerosis and CHD
- Hyperlipidemia and Dyslipidemia: Elevated levels of low-density lipoprotein (LDL) cholesterol, triglycerides, and low levels of high-density lipoprotein (HDL) cholesterol contribute to the formation of atherosclerotic plaques
- Diabetes Mellitus: Both type 1 and type 2 diabetes are associated with an increased risk of CHD. Diabetes accelerates atherosclerosis and impairs cardiovascular function
- Smoking: Cigarette smoking damages the endothelium, promotes inflammation, reduces HDL cholesterol, and increases platelet aggregation, all of which contribute to the development of CHD
- Obesity and Sedentary Lifestyle: Excessive body weight, particularly abdominal obesity, and a sedentary lifestyle are associated with increased insulin resistance, dyslipidemia, hypertension, and inflammation, all of which raise the risk of CHD
Non-modifiable risk Factors
- Age and Gender: The risk of CHD increases with age, with men being more susceptible to CHD than premenopausal women. However, after menopause the risk in women catches up due to hormonal changes
- Family History and Genetics: Having a first-degree relative (parent, sibling) with CHD increases the risk of developing the condition. Genetic factors also play a role in lipid metabolism and other biological processes related to CHD
- Ethnicity and Race: Certain ethnic groups, such as South Asians and African Americans, have a higher prevalence of CHD and associated risk factors
- Other Risk Factors
- Stress and Mental Health: Chronic stress, depression, and anxiety can contribute to the development and progression of CHD by affecting behavior, inflammation, and physiological processes
- Alcohol Consumption: Excessive alcohol consumption is associated with an increased risk of CHD. However, moderate alcohol intake may have a protective effect on the cardiovascular system
- Sleep Disorders: Sleep apnea and other sleep disorders are linked to an increased risk of hypertension, obesity, and metabolic disturbances, which can increase the risk of CHD
- By identifying and modifying modifiable risk factors through lifestyle changes, medication, and appropriate management of underlying conditions, it is possible to reduce the risk of developing CHD. Implementing preventive measures, such as maintaining a healthy weight, regular physical activity, following a balanced diet, managing stress, and avoiding smoking are key in mitigating the risk of CHD and improving overall cardiovascular health
How does coronary heart disease clinically manifest?
Clinical manifestations of coronary heart disease (CHD) can vary depending on the severity and extent of coronary artery blockage or narrowing. The two main clinical presentations of CHD are stable angina and acute coronary syndrome (ACS).
Stable angina
Stable angina is the most common manifestation of CHD and is characterized by episodes of chest pain or discomfort that occur predictably during physical exertion or emotional stress. Key features include:
- Chest pain or discomfort: Typically described as a pressure, tightness, squeezing, or burning sensation in the chest. The pain may radiate to the left arm, neck, jaw, or back
- Triggers: Chest pain is often triggered by physical activity, emotional stress, or exposure to cold temperatures
- Duration and relief: The pain usually lasts a few minutes (typically less than 10 minutes) and is relieved by rest or nitroglycerin medication
- Stable pattern: The frequency, intensity, and duration of angina episodes tend to remain consistent over time
Acute coronary syndrome (ACS)
ACS encompasses two conditions: unstable angina and myocardial infarction (MI). ACS represents a more critical and potentially life-threatening manifestation of CHD. The key features of ACS include:
Unstable Angina:
- Chest pain or discomfort: Similar to stable angina, but the pain may occur at rest or with minimal exertion
- Increased frequency and severity: Unstable angina episodes may become more frequent, prolonged, or severe compared to stable angina
- Unpredictable pattern: Unstable angina can occur unpredictably, even at rest, and is not always relieved by rest or nitroglycerin. It may be a warning sign of an impending heart attack
Myocardial infarction (heart attack):
- Complete coronary artery blockage: A blood clot forms on a ruptured atherosclerotic plaque, completely obstructing the coronary artery and causing a significant reduction in blood flow to a portion of the heart muscle
- Prolonged ischemia: Without prompt medical intervention, the affected heart muscle undergoes irreversible damage due to the lack of oxygen and nutrients
- Clinical presentation: Severe chest pain: Intense, prolonged chest pain that may radiate to the left arm, jaw, neck, or back. The pain is often described as crushing or squeezing, shortness of breath, difficulty breathing or feeling breathless even at rest or with minimal exertion; profound weakness or fatigue; sweating, lightheadedness, or nausea. Women and older adults may present with atypical symptoms such as indigestion, fatigue, or shortness of breath without chest pain
It is important to note that some individuals, particularly those with diabetes or older adults, may experience silent ischemia, where they have a lack of typical symptoms even during a heart attack. Hence, it is essential to be aware of other signs such as unexplained fatigue, shortness of breath, or indigestion.
Prompt recognition and medical attention are crucial for individuals experiencing symptoms of ACS, as it represents a medical emergency that requires immediate treatment to restore blood flow to the affected heart muscle.
Other manifestations of advanced CHD include heart failure, arrhythmias, and sudden cardiac death. These complications can occur due to the long-term effects of reduced blood supply to the heart muscle and the resultant cardiac remodeling.
Early diagnosis, timely intervention, and appropriate management of CHD are vital in preventing complications and improving outcomes for individuals with this condition. Regular cardiovascular assessments, including risk factor evaluation can aid in identifying individuals at risk for CHD and implementing preventive measures.
How is coronary heart disease diagnosed?
The diagnosis of coronary heart disease (CHD) involves a comprehensive evaluation that combines clinical assessment, medical history, physical examination, and various diagnostic tests. The goal is to determine the presence, severity, and extent of coronary artery disease. Below are the common methods for diagnosing CHD:
Medical History and Physical Examination
- The healthcare provider will gather information about the patient’s symptoms, risk factors, and medical history. They will ask about any chest pain or discomfort, shortness of breath, fatigue, or other cardiac-related symptoms
- A physical examination may be performed to assess vital signs, heart sounds, and signs of heart failure or other cardiac abnormalities
Electrocardiogram (ECG)
- An ECG records the electrical activity of the heart and can help identify irregularities in heart rhythm (arrhythmias) and signs of ischemia or previous heart attacks
- A resting ECG is typically the initial test performed and can provide important initial information. However, it may not always show abnormalities in the early stages of CHD
Exercise stress test
- This test assesses the heart’s response to physical stress and helps evaluate symptoms of CHD, such as chest pain or shortness of breath during exertion
- The patient exercises on a treadmill or stationary bike while connected to an ECG machine. The ECG readings are monitored for any changes indicative of reduced blood flow to the heart
Imaging Tests
- Echocardiogram: This ultrasound-based test uses sound waves to create images of the heart’s structure and function. It can help assess the pumping ability of the heart and detect abnormalities in the heart valves or wall motion
- Nuclear Stress Test: This test combines exercise or medication-induced stress with the injection of a radioactive tracer. Images are taken before and after stress to evaluate blood flow to the heart muscle
- Coronary Computed Tomography Angiography (CCTA): This non-invasive imaging technique uses a computed tomography (CT) scanner to visualize the coronary arteries and detect any narrowing or blockages
- Cardiac Magnetic Resonance Imaging (MRI): This imaging technique uses a magnetic field and radio waves to produce detailed images of the heart, helping assess cardiac structure, function, and blood flow
Invasive coronary angiography
- This is considered the gold standard for diagnosing CHD. It involves the insertion of a catheter into the coronary arteries to inject a contrast dye. X-ray images are then taken to visualize the blood flow and identify any blockages
- In some cases, during coronary angiography, additional procedures such as percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) may be performed to treat any identified blockages
Blood tests
Blood tests can help evaluate the levels of cholesterol, triglycerides, and other lipids that are associated with CHD. They can also measure cardiac enzymes or biomarkers released during a heart attack. The diagnostic approach for CHD varies based on the patient’s symptoms, risk factors, and the suspected severity of the disease. The choice of diagnostic tests is made by the healthcare provider, considering the individual patient’s needs and circumstances.
What are the treatment options for coronary heart disease?
The treatment of coronary heart disease (CHD) aims to relieve symptoms, reduce the risk of complications, and improve overall cardiovascular health. The specific treatment options depend on the severity of the disease, the presence of symptoms, and individual patient characteristics. Here are the key treatment modalities for CHD.
Lifestyle modifications
- Healthy Diet: A heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and low-fat dairy products is recommended. It should be low in saturated and trans fats, cholesterol, sodium, and added sugars
- Regular Exercise: Engaging in moderate aerobic exercise for at least 150 minutes per week, as recommended by healthcare professionals, helps improve cardiovascular fitness and overall health
- Smoking Cessation: Quitting smoking is crucial to reduce the risk of complications and slow the progression of CHD. Smoking cessation programs, medications, and counseling can be helpful
- Weight Management: Achieving and maintaining a healthy weight through a combination of healthy eating and regular physical activity is beneficial for individuals with CHD
Medications
- Antiplatelet Agents: Medications such as aspirin and clopidogrel are prescribed to prevent blood clot formation and reduce the risk of heart attack or stroke
- Cholesterol-Lowering Medications: Statins are commonly used to lower LDL cholesterol levels and reduce the risk of plaque formation and progression. Other medications, such as ezetimibe and PCSK9 inhibitors, may be used in combination or as alternatives
- Blood Pressure Control: Medications like beta-blockers, ACE inhibitors, angiotensin II receptor blockers (ARBs), and calcium channel blockers are used to manage hypertension and reduce the workload on the heart
- Nitroglycerin: Nitroglycerin helps relieve angina symptoms by relaxing and widening the coronary arteries, and improving blood flow to the heart
- Other Medications: Additional medications may be prescribed to manage specific symptoms or comorbidities, such as antiarrhythmics for irregular heart rhythms, anticoagulants for individuals with atrial fibrillation, or a high risk of blood clot formation
Invasive Procedures and Surgeries
- Percutaneous Coronary Intervention (PCI): This procedure involves the use of a catheter to open narrowed or blocked coronary arteries. It may include balloon angioplasty to widen the artery and stent placement to keep it open
- Coronary Artery Bypass Grafting (CABG): In cases where multiple coronary arteries are significantly blocked, bypass surgery may be recommended. It involves using blood vessels (usually from the leg or chest) to bypass the blocked arteries and restore blood flow to the heart muscle
Cardiac rehabilitation
Cardiac rehabilitation programs offer supervised exercise training, education, counseling, and support to individuals with CHD. These programs help improve cardiovascular fitness, manage risk factors, and promote a healthy lifestyle.
Psychological support
Psychological support, including counseling and stress management techniques, can help individuals cope with the emotional and psychological impact of CHD.
It is important to note that treatment plans are personalized based on the individual’s specific condition, risk factors, and preferences. Regular follow-up appointments with healthcare providers are essential to monitor progress, adjust medications, and modify treatment strategies as needed.
Prevention and early intervention play a significant role in managing CHD. Adopting a heart-healthy lifestyle, controlling risk factors, and seeking medical care promptly can help reduce the risk of complications and improve outcomes for individuals with CHD.
What medications are used in coronary heart disease?
Antiplatelet Medications
- Aspirin. Helps prevent blood clot formation by reducing platelet aggregation
- Clopidogrel. Another anti-platelet medication used to reduce the risk of blood clots
Statins
- Atorvastatin
- Simvastatin
- Rosuvastatin
- Pravastatin
- Lovastatin
- Fluvastatin
Beta-Blockers
- Metoprolol
- Atenolol
- Bisoprolol
- Propranolol
- Carvedilol
ACE Inhibitors (Angiotensin-Converting Enzyme Inhibitors)
- Lisinopril
- Enalapril
- Ramipril
- Quinapril
ARBs (Angiotensin II Receptor Blockers)
- Losartan
- Valsartan
- Irbesartan
- Candesartan
Calcium Channel Blockers (CCBs)
- Amlodipine
- Diltiazem
- Verapamil
Nitrates
- Nitroglycerin
- Isosorbide dinitrate
- Isosorbide mononitrate
Antiarrhythmic Medications
- Amiodarone
- Dronedarone
- Sotalol
What are the prevention strategies for coronary heart disease?
Prevention strategies for coronary heart disease (CHD) focus on reducing risk factors and adopting a heart-healthy lifestyle. By implementing these strategies, individuals can significantly lower their risk of developing CHD.
Healthy diet
- Consume a balanced diet: Include a variety of fruits, vegetables, whole grains, lean proteins, and low-fat dairy products in your diet
- Limit unhealthy fats: Reduce saturated and trans fats found in red meat, full-fat dairy products, fried foods, and processed snacks
- Minimize sodium intake: Limit the consumption of high-sodium foods, such as processed and packaged foods, and opt for fresh ingredients instead
- Control portion sizes: Maintain appropriate portion sizes to prevent overeating and excessive calorie intake
- Limit added sugars: Reduce the consumption of sugary beverages, sweets, and desserts
- Choose healthier cooking methods: Opt for baking, grilling, steaming, or sautéing instead of frying
Regular physical activity
- Engage in regular aerobic exercise: Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, such as brisk walking, swimming, cycling, or dancing
- Include strength training: Incorporate strength training exercises at least twice a week to improve muscle strength and overall fitness
- Be physically active throughout the day: Avoid prolonged sitting and find opportunities to be active during daily routines
Tobacco and alcohol use
- Quit smoking: Smoking is a significant risk factor for CHD. Seek support from healthcare professionals, counseling programs, and medications to quit smoking
- Limit alcohol consumption: Moderate alcohol consumption (up to one drink per day for women and up to two drinks per day for men) is generally considered acceptable. However, excessive alcohol intake can increase the risk of CHD and other health problems
Maintain a healthy weight
- Achieve and maintain a healthy body weight: Aim for a body mass index (BMI) within the normal range (18.5 to 24.9)
- Focus on gradual weight loss: If overweight or obese, even a modest weight loss can significantly reduce the risk of CHD
Control blood pressure
- Monitor blood pressure regularly: High blood pressure increases the risk of CHD. Get your blood pressure checked regularly and work with your healthcare provider to manage it within the recommended range
- Adopt lifestyle modifications: Implement strategies such as reducing sodium intake, maintaining a healthy weight, exercising regularly, and managing stress to help control blood pressure
Manage diabetes
Keep blood sugar levels under control: For individuals with diabetes, managing blood sugar levels is essential to reduce the risk of CHD. Follow a healthy eating plan, exercise regularly, take medications as prescribed, and monitor blood sugar levels.
Manage cholesterol levels
- Monitor cholesterol levels: Have your cholesterol levels checked regularly, especially LDL cholesterol (“bad” cholesterol). Follow healthcare provider recommendations for cholesterol screening and management
- Adopt a heart-healthy diet: Limit saturated and trans fats in your diet and include foods rich in healthy fats (such as omega-3 fatty acids)
- Medications: In some cases, cholesterol-lowering medications (such as statins) may be prescribed to manage high cholesterol levels
Stress management
Practice stress-reducing techniques: Engage in activities that help manage stress, such as meditation, deep breathing exercises, yoga, or engaging in hobbies.
Regular health check-ups
Regularly visit healthcare providers for preventive check-ups and screenings to assess your overall cardiovascular health, detect any risk factors, and take appropriate actions. In the UK, the NHS offers all adults between 40 and 74 a check-up to spot early signs of stroke, kidney disease, coronary heart disease and Type 2 diabetes.
Education and awareness
Stay informed about heart disease risk factors, symptoms, and preventive strategies. Educate yourself and your loved ones about heart-healthy lifestyles and make informed choices. Prevention strategies for CHD involve a combination of healthy lifestyle choices, risk factor management, and regular medical care. By adopting these strategies, individuals can lower their risk of developing CHD and improve their overall cardiovascular health. It is important to consult with healthcare professionals for personalized advice and guidance based on individual risk factors and medical history.
Emerging research in coronary heart disease
Coronary heart disease (CHD) is a well-studied condition, and ongoing research continues to provide valuable insights into the understanding, prevention, and treatment of the disease.
Pharmacogenetics and precision medicine
- Genomic research aims to identify genetic variations that contribute to the risk of CHD. This can help in the development of personalized treatment strategies and targeted therapies
- Advances in genomic medicine are leading to the identification of novel genetic markers associated with CHD, which may aid in risk prediction and early detection
Biomarkers for risk assessment and prognosis
- Researchers are investigating new biomarkers that can help assess the risk of CHD and predict outcomes. High-sensitivity troponin assays and novel inflammatory markers are being explored for their potential in risk stratification and prognosis
- Biomarkers related to oxidative stress, endothelial dysfunction, and plaque instability are also being studied to improve risk assessment and guide treatment decisions
Imaging techniques
- Advanced imaging modalities are being developed to improve the detection and characterization of coronary artery disease. This includes the use of coronary computed tomography angiography (CCTA), cardiac magnetic resonance imaging (MRI), and positron emission tomography (PET) for more accurate assessment of plaque burden, composition, and inflammation
- Emerging imaging techniques also focus on non-invasive evaluation of endothelial function and myocardial perfusion, providing valuable information on early changes in the coronary vasculature
Novel therapies and interventions
- Research is underway to develop new therapeutic approaches for CHD. This includes investigating novel drug targets, such as agents that reduce inflammation, stabilize plaques, or promote plaque regression
- Emerging therapies include gene therapy, stem cell therapy, and tissue engineering approaches to repair damaged heart tissue and promote cardiac regeneration
- Advancements in minimally invasive techniques for percutaneous coronary intervention (PCI), such as bioresorbable stents and drug-coated balloons aim to improve long-term outcomes and reduce the risk of restenosis
Artificial intelligence and machine learning
- Artificial intelligence (AI) and machine learning techniques are being applied to analyze large datasets and identify patterns in CHD. These approaches can help predict outcomes, improve risk stratification, and enhance diagnostic accuracy
- AI algorithms are also being developed to aid in the interpretation of medical imaging, assisting in the early detection and characterization of coronary artery disease
Lifestyle interventions
Research continues to explore the effectiveness of lifestyle interventions in preventing and managing CHD. Studies are investigating the impact of specific dietary patterns (such as the Mediterranean diet), physical activity interventions, and behavioral interventions for smoking cessation and stress reduction.
Sex and gender differences
There is growing recognition of sex and gender differences in CHD, including differences in risk factors, presentation, and outcomes. Research is focused on understanding these disparities and developing tailored approaches to prevention and treatment.
Telemedicine and digital health
The use of telemedicine and digital health technologies is expanding in the field of CHD. Remote monitoring, mobile applications, and wearable devices are being explored to improve patient engagement, self-management, and long-term outcomes.
What coronary heart disease support organizations are there available to support me in the UK?
- British Heart Foundation (BHF): The British Heart Foundation is a leading charity organization in the UK dedicated to supporting individuals with heart and circulatory diseases, including CHD. They offer information resources, support services, a helpline, local support groups, and an online community
- Cardiomyopathy UK: Cardiomyopathy UK is a charity organization that supports individuals with various heart conditions, including CHD. They provide information resources, support services, a helpline, and opportunities for connecting with others who have similar conditions
What coronary heart disease support organizations are there available to support me in the US?
- American Heart Association (AHA): The American Heart Association is a national organization dedicated to promoting heart health and preventing cardiovascular diseases, including CHD. They offer resources, educational materials, support groups, lifestyle tips, and advocacy initiatives
- Mended Hearts: Mended Hearts is a national nonprofit organization that provides support to individuals with heart disease, including CHD, and their caregivers. They offer hospital visitation programs, support groups, educational materials, and resources
- WomenHeart: The National Coalition for Women with Heart Disease: WomenHeart focuses specifically on women with heart disease, including CHD. They provide support, education, resources, and advocacy initiatives to empower women and promote heart health
- National Heart, Lung, and Blood Institute (NHLBI): The NHLBI is part of the National Institutes of Health (NIH) and provides resources and educational materials on various heart-related conditions, including CHD. Their website offers information on prevention, treatment, and lifestyle management
- Cardiac Rehabilitation: Cardiac rehabilitation programs are available in various hospitals and healthcare centers throughout the US. These programs provide support, education, and exercise training for individuals recovering from CHD events or managing their condition. They are usually supervised by a multidisciplinary team of healthcare professionals, including nurses, physiotherapists, and dietitians
- The Centers for Disease Control and Prevention
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.