Coronary heart disease (CHD) is a leading cause of death in both men and women in the UK, according to the NHS. However, with early detection and treatment, many people with coronary heart disease can live long healthy lives. Let’s take a look at what coronary heart disease is, its causes and treatment.
Let’s begin by understanding the heart. The heart is a muscle that pumps blood throughout the body. The blood carries oxygen and nutrients to all the cells of the body. The heart is like a pump that has four chambers, two on the right side and two on the left side. The right side of the heart has two chambers, called the right atrium and right ventricle. The left side of the heart also has two chambers, called the left atrium and left ventricle.
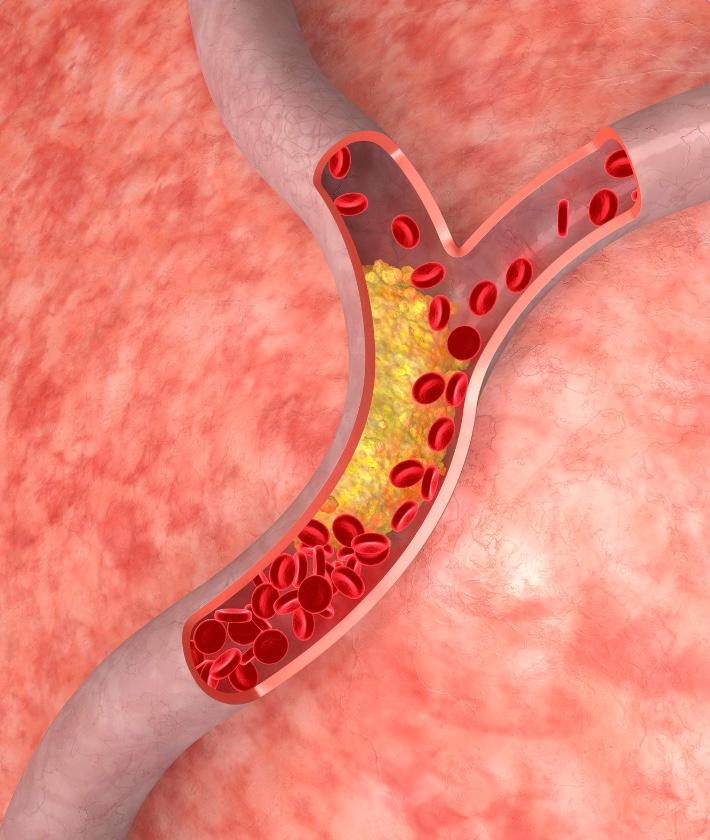
The coronary arteries are blood vessels that go from the aorta (a large vessel that comes off the left ventricle) to the heart muscle. These arteries supply oxygen-rich blood to the heart muscle.
Coronary heart disease is also known as ischaemic heart disease. It is a type of heart disease that occurs when these arteries become narrow or blocked due to a build-up of fatty deposits of plaque. Plaque is made up of fat, cholesterol, calcium and other substances found in the blood. When plaque builds up in an artery, it is called atherosclerosis.
Atherosclerosis makes it hard for blood to flow through your arteries. This can cause chest pain (angina), shortness of breath or a heart attack. A heart attack happens when plaque buildup in an artery cuts off or blocks blood flow to part of your heart muscle. When this happens, your heart muscle doesn’t get enough oxygen and begins to die.
Types of Coronary Heart Disease
There are different types of coronary artery diseases:
- Stable angina: This is chest pain or discomfort that happens when your heart muscle isn’t getting enough oxygen-rich blood. This usually happens during physical activity or emotional stress. The pain usually goes away with rest or medicine within 5 minutes
- Unstable angina: This is a more serious type of angina that can happen without physical activity or emotional stress. It may happen more often and last longer than stable angina. It can also occur at rest and be severe enough to wake you from sleep. Unstable angina could lead to a heart attack if not treated right away
- Myocardial infarction (heart attack): A heart attack happens when one of your coronary arteries becomes blocked so that blood flow to part of your heart muscle diminishes or stops completely. Many times, this blockage is caused by a clot (ischemic). If a person is showing symptoms of a heart attack, it is vital to call emergency services immediately
- Sudden cardiac death: Sometimes called sudden cardiac arrest or unexpected cardiac death. This happens when electrical impulses in your heart suddenly stop working properly causing your heart to beat dangerously fast or stop beating entirely. If this isn’t treated right away, it will lead to death within minutes
What are the symptoms of coronary heart disease?
Atherosclerosis is a gradual process that often has no symptoms for years before an event occurs. When plaque ruptures, a blood clot forms that can also block blood flow. If the clot is large enough, it can cause a heart attack. There are usually no signs or symptoms in the early stages of coronary heart disease. As it progresses, you may experience chest pain or discomfort called angina which is the most common symptom. Some people mistake it for heartburn or indigestion. This type of pain usually happens during physical activity because your heart isn’t getting enough oxygen-rich blood when you exert yourself.
Angina feels like tightness or squeezing in your chest that may also spread to your shoulders, arms, neck, jaw or back. If you have angina at rest or if it lasts longer than a few minutes at a time, it may be a sign of an impending heart attack and you should call emergency services right away. Other symptoms may include shortness of breath, lightheadedness or dizziness, nausea or vomiting, sweating and extreme fatigue (feeling tired all the time).
Not everyone experiences the same symptoms in the same way. Some people who have atherosclerosis don’t have any symptoms at all until they have a sudden cardiac event such as a heart attack or stroke.
What are the risk factors for Coronary Heart Disease?
Many factors can increase your risk of developing coronary heart disease. Some of these factors you can control and others you cannot. You can control some of the risk factors by making lifestyle changes to improve your heart health such as exercising regularly, eating a healthy diet and not smoking. Other risk factors include:
- High blood pressure (hypertension): Having high blood pressure puts extra strain on your arteries and heart. This increases your risk for coronary heart disease
- High cholesterol: High blood cholesterol levels specifically, serum LDL (low-density lipoprotein cholesterol) concentrations can cause plaque to build up in your arteries and increase your risk for coronary heart disease
- Smoking: Cigarette smoking damages your arteries and puts you at a higher risk for coronary heart disease
- Obesity/being overweight: Being overweight or obese puts extra strain on your arteries and increases your risk for coronary heart disease
- Unhealthy diet: Eating a diet high in saturated fats, trans fats, and sodium can increase your risk for coronary heart disease
- Sedentary lifestyle: A sedentary lifestyle can lead to obesity and increase your risk for coronary heart disease
- Family history: If you have a family member with coronary artery disease, you may have a higher risk for the condition yourself
- Age: Your risk for coronary artery disease increases as you age. This is because plaque buildup takes many years to occur
- Diabetes: Having diabetes means that you have high levels of blood sugar, which can damage your arteries and increase your risk of developing coronary artery disease
- Sleep apnea: Sleep apnea is a condition where you stop breathing while you are asleep. It can put extra strain on your cardiovascular system and raise your risk of heart disease and high blood pressure
- Chronic stress: Chronic stress can damage the lining of your arteries, making plaque more likely to develop
- Alcohol abuse: Drinking too much alcohol can raise your triglyceride levels and damage the lining of your arteries
- Illegal drug use: Using illegal drugs such as cocaine constricts blood vessels and raises the risks of developing coronary artery disease
- Adrenal gland disorders: Diseases affecting the adrenal glands (such as Cushing’s syndrome) can lead to an increase in cortisol levels; high cortisol levels are associated with an increased risk of developing cardiovascular diseases such as coronary artery disease
- Certain chronic illnesses and other health conditions: Conditions such as cancer, rheumatoid arthritis, psoriasis and end-stage kidney disease can increase risk
- Taking certain medications: Medications such as birth control pills, hormone replacement therapy, psychoactive medications, anabolic steroids and certain cancer treatments
How is coronary heart disease diagnosed?
Your doctor will initially look at your family and medical history, do a physical examination and order routine blood tests. CHD is typically diagnosed using a combination of coronary angiograms, electrocardiograms (ECGs), stress tests and echocardiograms.
An angiogram is an x-ray of the arteries that helps to show any blockages. An ECG is a test that measures the electrical activity of the heart and can indicate if there is any damage to the heart muscle. A stress test involves walking on a treadmill while hooked up to an ECG machine. This test monitors blood flow to the heart, heart rhythm and blood pressure during exercise. An echocardiogram uses sound waves to create images of the heart and can be used to look for any areas of damage. A CT scan may also be ordered to get a more detailed view of the arteries.
How is coronary heart disease treated?
CHD is a serious condition that requires prompt treatment. There are two main types of treatment for coronary heart disease: lifestyle changes and medical interventions. Lifestyle changes include quitting smoking, regular exercise, keeping a healthy weight, eating a healthy diet and managing stress. Medical interventions include commonly prescribed medications such as beta-blockers, blood-thinning medicines, ACE inhibitors and statins. In severe cases, undergoing surgery such as angioplasty, coronary artery bypass surgery or receiving a pacemaker.
Angioplasty
Coronary angioplasty is a minimally invasive heart procedure, also known as a percutaneous coronary intervention. It is used to improve blood flow to the heart. It is typically performed during a heart catheterisation, in which a long, thin tube called a catheter is inserted into the body through an incision in the groin. The catheter is then threaded through the arteries to the heart. Once in place, a small balloon is inflated at the tip of the catheter. This expands the artery and improves blood flow. In some cases, a stent may also be placed during angioplasty. A stent is a small, metal mesh tube that helps to keep the artery open and improve blood flow. Angioplasty is often used to treat coronary artery disease, and it can be performed on an emergency basis if someone is having a heart attack. The procedure typically takes less than an hour to complete and most people can go home the same day. Recovery time varies from person to person, but most people can resume normal activities within a few days.
Coronary artery bypass surgery
Coronary artery bypass surgery also called heart bypass surgery or coronary artery bypass graft (CABG) surgery, is a procedure used to correct a narrowed or blocked artery. The goal of this surgery is to improve blood flow and oxygen to the heart. During the procedure, a surgeon takes a healthy section of a blood vessel from another area in your body and attaches it to the blocked coronary artery. This creates a new path for blood to flow around the blockage. In some cases more than one bypass graft may be needed.
Pacemaker
A pacemaker is a small device that is placed under the skin on the chest. The pacemaker sends electrical impulses to the heart muscle, which helps the heart to pump blood more effectively. Pacemaker therapy can improve quality of life and reduce your risk of developing CHD-related complications, such as heart failure. In some cases, pacemaker therapy may also be used to treat other heart conditions, such as arrhythmias.
Coronary heart disease is a serious condition that affects millions of people worldwide every year. While some risk factors are out of our control, such as family history, there are many things we can do to lower our risks, such as making healthy lifestyle choices. If you think you may be at risk for coronary artery disease or if you already have the condition talk to your doctor about ways you can lower your risks and prevent further damage to your heart muscle. By working together with our healthcare providers, we can all take steps towards reducing our risks for developing this condition – and improving our overall cardiovascular health!
Sources
- Coronary Angiography – NHS
- Coronary Artery Disease (CAD) – CDC
- Coronary heart disease – NHS
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.