High Cholesterol
Get valuable insights into High Cholesterol, including its causes, symptoms, prevention strategies, and treatment options, while also learning about how you can lower the cost of the medications used to treat High Cholesterol.
MEDICAL INFORMATION
High Cholesterol Key Facts
Related Medications
High cholesterol is a prevalent health condition that affects millions of people worldwide. While cholesterol is necessary for various bodily functions, an excess of it can lead to significant health risks. Here, we aim to provide you with an in-depth overview of the causes, effects, and management of high cholesterol, as well as the importance of maintaining healthy cholesterol levels.
What is the definition of high cholesterol?
High cholesterol refers to elevated levels of cholesterol in the blood. Cholesterol is a fatty substance that is essential for the body’s normal functioning, but excessive levels of certain types of cholesterol can increase the risk of developing cardiovascular diseases, such as heart disease and stroke.
What are the causes and risk factors associated with high cholesterol?
High cholesterol can be influenced by a combination of genetic and lifestyle factors. The causes and risk factors associated with high cholesterol include:
Poor Diet
Consuming a diet high in saturated fats and trans fats, found in foods such as red meat, full-fat dairy products, fried foods, and commercially baked goods, can raise LDL cholesterol levels.
Sedentary Lifestyle
Lack of regular physical activity can contribute to higher LDL cholesterol levels and lower HDL cholesterol levels. Exercise helps raise HDL cholesterol and improve overall cardiovascular health.
Obesity
Being overweight or obese increases the production of LDL cholesterol and decreases HDL cholesterol. Excess weight can also lead to other risk factors, such as high blood pressure and insulin resistance.
Genetics and Family History
Genetic factors play a role in cholesterol levels. Certain genetic conditions, such as familial hypercholesterolemia, can cause very high LDL cholesterol levels from birth. Family history of high cholesterol or early heart disease can also increase the risk.
Age and Gender
Cholesterol levels tend to rise with age, as the body’s metabolism changes. Men typically have higher cholesterol levels than premenopausal women. However, after menopause, women’s LDL cholesterol levels often increase.
Smoking
Smoking damages blood vessels and lowers HDL cholesterol levels. It also increases the risk of developing atherosclerosis and heart disease.
Diabetes
High blood sugar levels in diabetes can lower HDL cholesterol and raise LDL cholesterol and triglyceride levels.
Certain Medical Conditions
Underlying conditions, such as chronic kidney disease, hypothyroidism, and liver diseases, can impact cholesterol levels.
Medications and Hormonal Conditions
Certain medications, such as corticosteroids, diuretics, and some immunosuppressants, can affect cholesterol levels. Hormonal conditions like polycystic ovary syndrome (PCOS) and hypothyroidism can also contribute to high cholesterol.
Diet High in Cholesterol
Although dietary cholesterol has a smaller impact on blood cholesterol levels compared to saturated and trans fats, some individuals are more sensitive to dietary cholesterol intake.
What are the different types of cholesterol?
There are different types of cholesterol based on the type of lipoproteins that carry cholesterol in the bloodstream. The main types of cholesterol include:
Low-Density Lipoprotein (LDL) Cholesterol
LDL cholesterol is often referred to as “bad” cholesterol. It carries cholesterol from the liver to peripheral tissues and organs. If there is an excess of LDL particles or impaired LDL receptor function, LDL cholesterol can accumulate in the arterial walls, leading to atherosclerosis and an increased risk of cardiovascular disease.
High-Density Lipoprotein (HDL) Cholesterol
HDL cholesterol is often referred to as “good” cholesterol. HDL particles help remove excess cholesterol from the bloodstream and arterial walls, transporting it back to the liver for excretion or reuse. High levels of HDL cholesterol are considered beneficial as they can help protect against heart disease.
Triglycerides
Triglycerides are a type of fat found in the blood. They are produced by the liver and obtained through the consumption of fatty foods. High levels of triglycerides are often associated with high LDL cholesterol levels and low HDL cholesterol levels. Elevated triglycerides can also contribute to atherosclerosis and increase the risk of cardiovascular disease.
Total Cholesterol
Total cholesterol refers to the sum of LDL cholesterol, HDL cholesterol, and a fraction of triglycerides in the bloodstream. It provides an overall assessment of cholesterol levels but does not provide information about the distribution of LDL and HDL cholesterol. It’s important to note that the ratio between LDL and HDL cholesterol, as well as the absolute levels of LDL cholesterol and HDL cholesterol, are significant factors in assessing the risk of cardiovascular disease. A lipid profile blood test is typically performed to measure these cholesterol components and triglyceride levels.
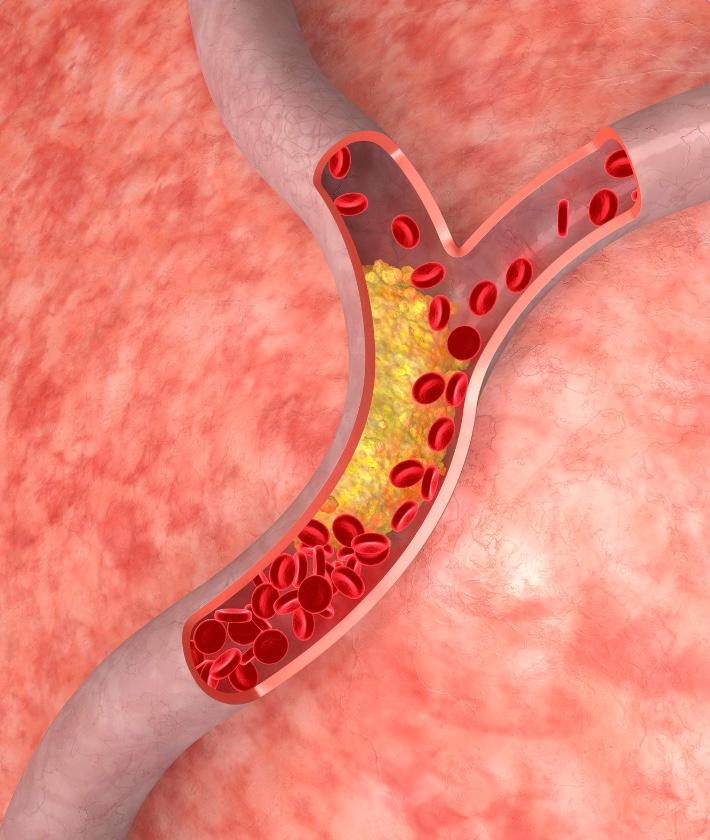
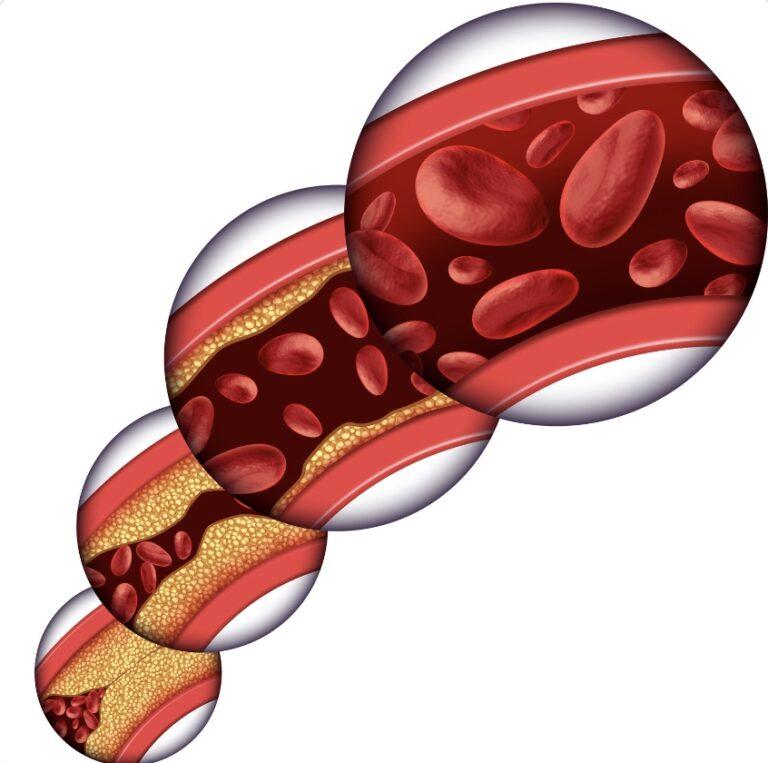
What is the pathophysiology of high cholesterol?
The pathophysiology of high cholesterol, specifically elevated levels of low-density lipoprotein (LDL) cholesterol, involves the complex interplay of various factors in the body. Here’s a general overview:
- Cholesterol production: Cholesterol is a waxy substance produced by the liver and is also obtained through the diet. The liver synthesizes cholesterol based on the body’s needs
- Lipoprotein transport: Cholesterol is transported in the bloodstream as lipoproteins. LDL cholesterol is known as “bad” cholesterol because it carries cholesterol from the liver to peripheral tissues, including the arterial walls
- LDL receptor interaction: Normally, cells in the body have LDL receptors on their surfaces, which bind to LDL particles and facilitate their uptake into the cells. However, in individuals with high cholesterol, there may be an overproduction of LDL or a reduced number of LDL receptors, leading to an accumulation of LDL particles in the blood
- Arterial deposition: When LDL cholesterol levels are elevated, LDL particles can penetrate the endothelial lining of blood vessels and accumulate within the arterial walls. This process triggers an inflammatory response
- Formation of plaques: Over time, the accumulated LDL cholesterol undergoes modifications, attracting immune cells (such as macrophages) to the arterial walls. The immune cells engulf the LDL particles, forming foam cells. These foam cells contribute to the formation of fatty plaques, leading to a condition called atherosclerosis
- Narrowing of arteries: As the plaques grow and accumulate, they harden and narrow the arteries. This process, called stenosis, restricts blood flow to vital organs, including the heart and brain
- Complications: If an atherosclerotic plaque ruptures, it can trigger the formation of a blood clot, which can partially or completely block the blood flow to the affected area. This can result in various cardiovascular complications, such as heart attack or stroke
It’s important to note that other factors, such as genetics, diet, lifestyle, and underlying medical conditions, can also influence cholesterol metabolism and contribute to high cholesterol levels. Managing high cholesterol often involves a combination of lifestyle modifications (e.g., healthy diet, regular exercise) and, in some cases, medications to control cholesterol levels and reduce the risk of complications.
What are the signs and symptoms of high cholesterol?
High cholesterol does not typically cause any noticeable signs or symptoms on its own. It is a silent condition that often goes undiagnosed until it leads to complications such as heart disease or stroke. That’s why it’s important to have your cholesterol levels checked regularly, especially if you have risk factors such as a family history of high cholesterol, a sedentary lifestyle, obesity, or a poor diet.
However, in some cases, high cholesterol can manifest as a condition called xanthomas. Xanthomas are fatty deposits that build up under the skin, typically around the eyes, elbows, knees, or tendons. These deposits appear as yellowish bumps or lumps and may be an indication of high cholesterol levels. It’s worth noting that the only definitive way to diagnose high cholesterol is through a blood test called a lipid profile. This test measures different types of cholesterol and triglycerides in your blood.
If you’re concerned about your cholesterol levels or experiencing any related symptoms, it’s essential to consult a healthcare professional for proper evaluation and guidance. They can assess your risk factors, order appropriate tests, and provide personalized recommendations to manage your cholesterol levels effectively.
What is the classification of high cholesterol (UK)?
In the United Kingdom, high cholesterol levels are typically categorized into different stages based on the levels of total cholesterol and LDL cholesterol. The stages of high cholesterol in the UK are generally defined as follows:
Desirable (UK)
- Total cholesterol: Below 5.0 mmol/L
- LDL cholesterol: Below 3.0 mmol/L
Borderline High (UK)
- Total cholesterol: 5.0-6.4 mmol/L
- LDL cholesterol: 3.0-4.0 mmol/L
High (UK)
- Total cholesterol: 6.5 mmol/L and above
- LDL cholesterol: 4.0 mmol/L and above
It’s important to note that these values are general guidelines, and healthcare professionals may take into consideration additional factors such as age, overall health, and the presence of other risk factors when assessing cholesterol levels and determining appropriate treatment or management strategies. In addition to total cholesterol and LDL cholesterol, other lipid parameters like HDL cholesterol and triglyceride levels are also considered when evaluating overall cardiovascular risk. A comprehensive lipid profile blood test is typically conducted to assess these parameters and provide a more detailed analysis of an individual’s cholesterol profile. It’s worth noting that the specific ranges and categorizations may vary slightly between different countries or healthcare organizations, so it’s always best to consult with a healthcare professional for personalized guidance and interpretation of cholesterol levels.
What is the classification of high cholesterol (US)?
In the United States, high cholesterol levels are typically categorized into different stages based on the levels of total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides. The stages of high cholesterol in the US are generally defined as follows:
Desirable (US)
- Total cholesterol: Below 200 mg/dL
- LDL cholesterol: Below 100 mg/dL
- HDL cholesterol: Above 60 mg/dL
- Triglycerides: Below 150 mg/dL
Borderline High (US)
- Total cholesterol: 200-239 mg/dL
- LDL cholesterol: 130-159 mg/dL
- HDL cholesterol: 40-59 mg/dL
- Triglycerides: 150-199 mg/dL
High (US)
- Total cholesterol: 240 mg/dL and above
- LDL cholesterol: 160 mg/dL and above
- HDL cholesterol: Below 40 mg/dL (considered a risk factor)
- Triglycerides: 200-499 mg/dL
Very High (US)
- Triglycerides: 500 mg/dL and above
It’s important to note that these values are general guidelines, and healthcare professionals may consider additional factors such as age, overall health, and the presence of other risk factors when evaluating cholesterol levels and determining appropriate treatment or management strategies.
It’s worth mentioning that the specific ranges and categorizations may vary slightly between different guidelines and healthcare organizations. Therefore, it’s always best to consult with a healthcare professional for personalized guidance and interpretation of cholesterol levels based on the specific guidelines followed in your country or healthcare system.
Does ethnicity play a role in high cholesterol?
Ethnicity can play a role in the prevalence and risk of high cholesterol. Different ethnic groups may have varying rates of high cholesterol and associated cardiovascular diseases.
South Asians
South Asians, including individuals of Indian, Pakistani, Bangladeshi, and Sri Lankan descent, tend to have higher rates of high cholesterol and a higher risk of heart disease compared to other ethnic groups. They often have a higher prevalence of small, dense LDL particles, which are considered more atherogenic (likely to contribute to the development of atherosclerosis).
African Americans
African Americans have a higher risk of high cholesterol and related complications, such as heart disease and stroke, compared to some other ethnic groups. They may also have lower levels of HDL cholesterol (the “good” cholesterol) and higher levels of triglycerides.
Hispanics/Latinos
Hispanics/Latinos, particularly those of Mexican, Puerto Rican, and Dominican descent, may have higher rates of high cholesterol and are at an increased risk of cardiovascular diseases. They may have higher levels of triglycerides and lower levels of HDL cholesterol.
Caucasians
Caucasians, also known as whites or individuals of European descent, can also develop high cholesterol and related conditions. The risk can vary within this ethnic group based on individual factors such as lifestyle, diet, and genetic predisposition. It’s important to remember that these ethnic variations are influenced by a combination of genetic, lifestyle, and environmental factors. Other factors such as socioeconomic status, cultural dietary habits, and healthcare disparities may also contribute to differences in high cholesterol prevalence and management among different ethnic groups.
How is high cholesterol diagnosed?
High cholesterol is typically diagnosed through a blood test called a lipid profile or lipid panel. This test measures the levels of different types of cholesterol and triglycerides in your blood. Below is an overview of the diagnostic process:
Discussion of risk factors
Your healthcare provider will assess your medical history, including any family history of high cholesterol or cardiovascular disease, as well as your lifestyle habits, such as diet, exercise, and smoking.
Fasting Requirement
To obtain accurate results, a lipid profile usually requires fasting for 9 to 12 hours before the blood sample is taken. This means avoiding food and drink (except water) during this period.
Blood Sample Collection
A healthcare professional will draw a blood sample, typically from a vein in your arm, using a needle. The sample is then sent to a laboratory for analysis.
Lipid profile results
The lipid profile test provides information about several lipid parameters, including total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides. These results will indicate the levels of each component in your blood.
Evaluation and Interpretation
Your healthcare provider will assess your lipid profile results, taking into consideration your overall health, risk factors, and established guidelines. They will determine whether your cholesterol levels are within a healthy range or if further management or treatment is necessary.
It’s important to note that guidelines may vary slightly between different countries or healthcare organizations, so the specific target levels and treatment recommendations may differ. Your healthcare provider will provide personalized recommendations based on your individual situation.
Regular cholesterol screenings are recommended, especially for individuals with risk factors or a family history of high cholesterol or cardiovascular disease. Early detection and management of high cholesterol can help reduce the risk of complications and support cardiovascular health.
How is high cholesterol prevented?
Preventing high cholesterol involves adopting a healthy lifestyle and making proactive choices to maintain optimal cholesterol levels. Here are some preventive measures:
Healthy Diet
- Choose a diet rich in fruits, vegetables, whole grains, and lean proteins
- Limit saturated fats found in red meat, full-fat dairy products, and fried foods
- Avoid trans fats found in processed and commercially baked goods
- Include sources of healthy fats, such as nuts, seeds, and fatty fish (like salmon)
- Limit dietary cholesterol by moderating the intake of high-cholesterol foods like organ meats and shellfish
Regular Physical Activity
- Engage in regular aerobic exercise, such as brisk walking, jogging, cycling, or swimming, for at least 150 minutes per week
- Include strength training exercises to improve overall fitness
- Consult with a healthcare professional before starting any exercise program, especially if you have underlying health conditions
Maintain a Healthy Weight
- Achieve and maintain a healthy weight through a combination of balanced diet and regular exercise
- Losing excess weight can help improve cholesterol levels and overall cardiovascular health
Avoid Smoking and Limit Alcohol Consumption
- Quit smoking or avoid tobacco use altogether, as it can lower HDL cholesterol and damage blood vessels
- Limit alcohol intake to moderate levels, as excessive alcohol consumption can raise triglyceride levels
Manage Diabetes and Hypertension
- Keep diabetes under control through proper management of blood sugar levels
- Control high blood pressure (hypertension) through lifestyle modifications, medications, or a combination of both, as it can contribute to high cholesterol levels
Regular Cholesterol Screenings
- Schedule regular check-ups with a healthcare professional and undergo cholesterol screenings as recommended based on your risk factors and guidelines
What are the treatment and management options for high cholesterol?
The treatment and management options for high cholesterol aim to reduce cholesterol levels, lower the risk of cardiovascular disease, and improve overall heart health. The specific approach may vary depending on an individual’s cholesterol levels, overall health, and other risk factors. Here are common treatment and management options:
Lifestyle Modifications
- Healthy Diet: Adopt a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit saturated fats, trans fats, and cholesterol in the diet
- Regular Exercise: Engage in aerobic exercise and strength training regularly. Aim for at least 150 minutes of moderate-intensity aerobic activity per week
- Weight Management: Maintain a healthy weight through a balanced diet and regular physical activity
- Smoking Cessation: Quit smoking or avoid tobacco use altogether
- Limit Alcohol Consumption: Moderate alcohol intake or avoid it altogether, depending on individual circumstances
Medications
- Statins: Statin medications are commonly prescribed to lower LDL cholesterol levels. They work by inhibiting an enzyme involved in cholesterol synthesis in the liver. Statins may also have other beneficial effects on cardiovascular health
- Other Medications: In some cases, additional medications, such as ezetimibe, bile acid sequestrants, or PCSK9 inhibitors, may be prescribed to further lower cholesterol levels or manage specific situations
- Combination Therapy: Depending on the individual’s condition, a combination of different medications may be recommended to achieve target cholesterol levels
Monitoring and Follow-up
- Regular Monitoring: Regular cholesterol screenings and follow-up appointments with a healthcare professional are important to assess the effectiveness of treatment and adjust management strategies as needed
- Lifestyle Maintenance: Continued adherence to healthy lifestyle habits is crucial for long-term cholesterol management and cardiovascular health
Management of Underlying Conditions
- If high cholesterol is associated with other medical conditions, such as diabetes or hypertension, it’s important to manage those conditions effectively through appropriate medications and lifestyle modifications
What medications are used in high cholesterol?
Statins
- Atorvastatin (Lipitor)
- Rosuvastatin (Crestor)
- Simvastatin (Zocor)
- Pravastatin (Pravachol)
- Lovastatin (Mevacor)
- Fluvastatin (Lescol)
Ezetimibe
- Ezetimibe (Zetia) works by reducing the absorption of cholesterol from the diet. It is often used in combination with statins
PCSK9 Inhibitors
- Alirocumab (Praluent)
- Evolocumab (Repatha) are injectable medications that can significantly lower LDL cholesterol levels. They are typically used for people with familial hypercholesterolemia or those who cannot tolerate statins
Bile Acid Sequestrants
- Colesevelam (Welchol)
- Cholestyramine (Questran) bind to bile acids in the intestines, reducing cholesterol absorption. They are often prescribed in combination with statins
Fibrates
- Fenofibrate (Tricor)
- Gemfibrozil (Lopid) can help lower triglyceride levels and raise HDL cholesterol. They are commonly used in individuals with high triglycerides
Niacin (Nicotinic Acid)
- Niacin (Niaspan) is a B vitamin that can raise HDL cholesterol and lower LDL cholesterol levels. It is often used in combination with other cholesterol-lowering medications
Omega-3 Fatty Acids
- Prescription-strength omega-3 fatty acid supplements, such as Vascepa, may be used to lower triglyceride levels in individuals with very high triglycerides
What are the complications of high cholesterol?
High cholesterol can lead to several complications, primarily related to the development of atherosclerosis, a condition characterized by the buildup of plaque in the arteries. The complications of high cholesterol include:
- Coronary Artery Disease (CAD): High cholesterol is a significant risk factor for CAD, which occurs when the arteries that supply blood to the heart become narrowed or blocked. This can lead to angina (chest pain), heart attack, or other serious heart conditions
- Stroke: Atherosclerosis can affect the arteries supplying blood to the brain, leading to reduced blood flow or a complete blockage, resulting in a stroke. High cholesterol increases the risk of developing ischemic strokes, which are caused by a lack of blood supply to the brain
- Peripheral Artery Disease (PAD): Atherosclerosis can also affect the arteries in the legs and other peripheral areas, leading to PAD. PAD can cause pain, cramping, and reduced circulation in the legs, increasing the risk of non-healing wounds and limb complications
- Aneurysms: Atherosclerosis weakens the arterial walls, increasing the risk of developing an aneurysm. An aneurysm is a bulge or enlargement of an artery that can rupture, causing severe internal bleeding and potentially life-threatening complications
- Hypertension: High cholesterol can contribute to the development of high blood pressure, which further strains the arteries and increases the risk of cardiovascular complications
- Metabolic Syndrome: High cholesterol is often associated with other conditions that collectively form metabolic syndrome. Metabolic syndrome includes high blood pressure, high blood sugar, excess abdominal fat, and abnormal cholesterol levels. Together, these factors significantly increase the risk of heart disease, stroke, and type 2 diabetes
- Gallstones: Elevated levels of cholesterol in the bile can contribute to the formation of gallstones, which can cause pain and other digestive complications
It’s important to note that the complications of high cholesterol are not immediate and usually develop over time. However, by managing cholesterol levels and adopting a heart-healthy lifestyle, the risk of these complications can be significantly reduced. Regular screenings, medical consultations, and adherence to treatment and lifestyle recommendations are essential for preventing and managing these complications.
Promising research and future direction of high cholesterol
Promising research and future directions in the field of high cholesterol focus on advancing our understanding of cholesterol metabolism, identifying novel therapeutic targets, and developing innovative treatment approaches. Here are some areas of research that show promise:
- PCSK9 Inhibitors: PCSK9 inhibitors (Evolocumab, Alirocumab) are a relatively new class of medications that lower LDL cholesterol by blocking the PCSK9 protein, which reduces the breakdown of LDL receptors. Ongoing research is focused on optimizing the use of PCSK9 inhibitors and exploring their long-term safety and effectiveness
- Targeting Triglycerides: High triglyceride levels are often associated with high cholesterol and cardiovascular risk. Research is underway to develop new therapies specifically targeting triglycerides, such as medications that inhibit key enzymes involved in triglyceride metabolism
- Gene Therapy and RNA-based Therapies: Gene therapy approaches are being investigated to correct genetic disorders that lead to high cholesterol, such as familial hypercholesterolemia. RNA-based therapies, including RNA interference and antisense oligonucleotides, are also being explored to target specific genes involved in cholesterol metabolism
- Novel Lipid-Lowering Agents: Researchers are working on the development of new medications and treatment approaches that can lower cholesterol levels effectively and safely. These include novel classes of drugs, such as ATP-citrate lyase inhibitors and agents that target the cholesterol absorption pathway
- Precision Medicine: Advancements in genetics and personalized medicine are enabling a more tailored approach to cholesterol management. Genetic profiling can identify individuals who may be more susceptible to high cholesterol or who may respond better to specific treatments, allowing for more personalized interventions
- Lifestyle Interventions and Digital Health: Research continues to emphasize the importance of lifestyle modifications in cholesterol management. Innovative approaches, such as digital health technologies, mobile apps, and wearable devices, are being developed to provide personalized guidance, monitoring, and support for individuals to make and sustain healthy lifestyle changes
- Public Health Initiatives: Public health efforts, including awareness campaigns, educational programs, and policy changes, are crucial for promoting healthy lifestyles, reducing dietary cholesterol intake, and encouraging regular cholesterol screenings. These initiatives aim to prevent and manage high cholesterol on a broader scale
What high cholesterol support organisations are there available to support me in the UK?
- British Heart Foundation (BHF). The British Heart Foundation is the largest cardiovascular charity in the UK. They provide a wide range of resources, information, and support for individuals with heart conditions, including high cholesterol. Their website offers helpful guidance on managing cholesterol, healthy eating, physical activity, and lifestyle changes
- HEART UK. HEART UK is a charity dedicated to supporting individuals with high cholesterol, familial hypercholesterolemia (FH), and related cardiovascular conditions. They provide resources, educational materials, and support for patients, their families, and healthcare professionals. Their website offers information on cholesterol management, diet, and lifestyle changes
- NHS Cholesterol Information. The National Health Service (NHS) in the UK provides comprehensive information and guidance on high cholesterol. Their website offers advice on understanding cholesterol levels, dietary recommendations, treatment options, and lifestyle modifications to reduce cholesterol
- Local NHS Services. Contacting your local NHS services, such as your GP (general practitioner) or community health clinics, can provide access to personalized support and guidance for managing high cholesterol. They can offer advice, perform cholesterol testing, and provide treatment options tailored to your specific needs
What high cholesterol support organisations are there available to support me in the US?
- American Heart Association (AHA). The American Heart Association is a leading organization dedicated to cardiovascular health. They provide resources, information, and support for individuals with high cholesterol. Their website offers educational materials, lifestyle recommendations, and guidance on managing cholesterol levels
- National Lipid Association (NLA). The NLA is a professional medical organization focused on advancing lipidology and improving patient care related to lipid disorders, including high cholesterol. Their website offers resources, patient education materials, and a directory to help find lipid specialists in your area
- FH Foundation. The FH Foundation is a nonprofit organization dedicated to raising awareness and improving the diagnosis and treatment of familial hypercholesterolemia (FH), a genetic condition that causes high cholesterol. They offer resources, support, and advocacy for individuals and families affected by FH
- Centers for Disease Control and Prevention (CDC). The CDC provides public health information and resources on high cholesterol and cardiovascular health. Their website offers educational materials, guidelines, and tools for managing cholesterol levels and reducing cardiovascular risk
- Local Support Groups and Community Health Centers. Local support groups and community health centers can provide valuable support and guidance for individuals with high cholesterol. These groups and centers may offer educational programs, counseling, and opportunities to connect with others facing similar challenges. Contact your local health department or community organizations to inquire about local support options
Summary
High cholesterol is a widespread health concern that requires attention and proactive management. By understanding the causes, effects, and management strategies, individuals can take control of their cholesterol levels and reduce the risk of associated complications. Regular check-ups, lifestyle modifications, and, if necessary, appropriate medications can help maintain healthy cholesterol levels and promote overall cardiovascular well-being. Consultation with healthcare professionals is crucial for personalized advice and guidance based on individual risk factors and medical history.
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.