Chronic Kidney Disease
Get valuable insights into Chronic Kidney Disease, including its causes, symptoms, prevention strategies, and treatment options, while also learning about how you can lower the cost of the medications used to treat Chronic Kidney Disease.

MEDICAL INFORMATION
Chronic Kidney Disease Key Facts
Related Medications
Chronic kidney disease (CKD) is a progressive and irreversible condition characterized by the gradual loss of kidney function. Here, we aim to provide you with an in-depth analysis of CKD by exploring its definition, etiology, risk factors, pathophysiology, clinical manifestations, diagnosis, treatment modalities, and management strategies. We highlight the importance of early detection, effective management, and lifestyle modifications in slowing disease progression and improving the quality of life for individuals with CKD.
What is the definition and stages of chronic kidney disease?
Chronic kidney disease (CKD) is a progressive condition characterized by the gradual loss of kidney function over time. The stages of kidney damage are classified based on the estimated glomerular filtration rate (eGFR), which measures how well the kidneys are filtering waste and fluid from the blood. The stages of kidney damage are commonly referred to as CKD stages and are as follows:
Stage 1: Kidney damage with normal or increased eGFR (≥90 ml/min)
In this early stage, there may be evidence of kidney damage, such as the presence of protein or blood in the urine, but the eGFR is normal or only slightly decreased. Patients in this stage often have few or no symptoms, and treatment aims to identify and address the underlying cause of kidney damage.
Stage 2: Mildly decreased eGFR (60-89 ml/min)
In stage 2, there is mild kidney damage with a slight decrease in eGFR. Kidney function is still relatively preserved, and patients may experience few or no symptoms. Treatment focuses on managing underlying conditions and adopting a healthy lifestyle to prevent further kidney damage.
Stage 3: Moderately decreased eGFR (30-59 ml/min)
Stage 3 is further divided into two sub-stages:
- Stage 3a: eGFR between 45-59 ml/min
- Stage 3b: eGFR between 30-44 ml/min
In stage 3, there is moderate kidney damage, and patients may start to experience symptoms such as fatigue, fluid retention, and changes in urine output. Sickness is also a symptom, since there is a build up of waste, because the kidneys cannot filter waste effectively leading to build up in the blood. Treatment involves managing complications, controlling blood pressure, and addressing underlying causes of kidney disease.
Stage 4: Severely decreased eGFR (15-29 ml/min)
In stage 4, kidney function is significantly impaired, and patients may experience more pronounced symptoms such as anemia, bone disease, and fluid overload. Treatment focuses on managing symptoms, slowing disease progression, and preparing for kidney replacement therapy, such as dialysis or kidney transplantation.
Stage 5: Kidney failure or end-stage renal disease (ESRD) (eGFR <15 ml/min)
In stage 5, the kidneys have lost nearly all their function, and patients require kidney replacement therapy to survive. Treatment options include dialysis or kidney transplantation. Symptom management, nutritional support, and psychological support are also essential components of care.
It’s important to note that the eGFR alone does not provide a complete picture of kidney health, and other factors such as the presence of albuminuria (protein in the urine) and underlying medical conditions are also considered in the assessment and management of CKD.
Early detection and management of kidney disease, along with appropriate lifestyle modifications and medical interventions can help slow the progression of kidney damage and improve outcomes for individuals with CKD. Regular monitoring and follow-up with healthcare providers are crucial for individuals at risk or diagnosed with CKD.
What are the causes of chronic kidney disease and what are the risk factors?
Several factors contribute to the development of CKD. This section explores the primary causes and risk factors, including diabetes mellitus, hypertension, glomerulonephritis, polycystic kidney disease, and other less common causes.
Diabetes Mellitus
Diabetes is the leading cause of CKD worldwide. There is a link between diabetes and CKD and the importance of glycemic control in preventing kidney complications. High blood sugar can damage the blood vessels in the kidneys. The damaged vessels can cause kidney damage.
Hypertension
High blood pressure is a significant risk factor for CKD. There is a relationship between hypertension and CKD and it is important to control blood pressure in preserving kidney function. High blood pressure, over time, can put a strain on the blood vessels in the kidneys and eventually stop of the kidneys working.
Glomerulonephritis
Glomerulonephritis refers to inflammation of the glomeruli, the filtering units of the kidneys. This subsection discusses the different types of glomerulonephritis and their impact on kidney function.
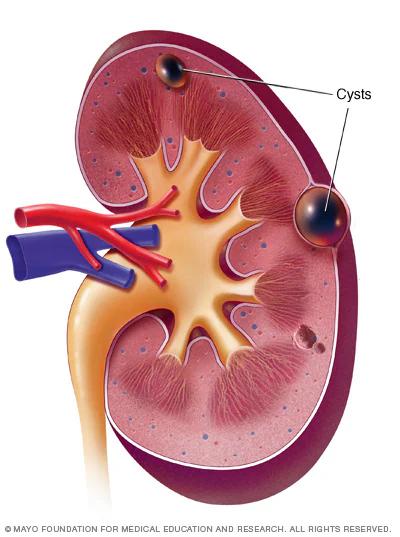
Polycystic Kidney Disease
Polycystic kidney disease is a genetic disorder characterized by the growth of fluid-filled cysts in the kidneys.
Hypocalcemia
Hypocalcemia in chronic renal failure is due to two primary causes:
- Decreased renal production of 1,25 (OH)2 vitamin D. Humans cannot make vitamin D. We can only get vitamin D from food and by exposing our skin to sunlight. Healthy kidneys can take that vitamin D we absorb and change it to an active form. That active vitamin D then helps us absorb calcium. But in chronic kidney disease (CKD), the kidneys are less able to make active vitamin D. Without enough active vitamin D, you absorb less calcium from the food you eat, so it then becomes low in your blood
- Increased serum phosphorus. Extra phosphorus in the blood of people with CKD may bind to calcium in the blood. This can then lower serum calcium
Other causes and risk factors
Less common causes of CKD include autoimmune diseases, kidney stones, recurrent kidney infections, urinary tract obstruction, and certain medications.
What is the pathophysiology of chronic kidney disease?
Understanding the pathophysiological processes involved in CKD is crucial for comprehending the disease’s progression. There is a clear impact of reduced glomerular filtration rate, renal blood flow, and renal tubular dysfunction on kidney function.
What are the clinical manifestations of chronic kidney disease?
The clinical manifestations of CKD can vary depending on the stage and severity of the disease. This section discusses the early and advanced signs and symptoms of CKD, including changes in urine output, fluid and electrolyte imbalances, anemia, bone disorders, and cardiovascular complications.
People with moderate to severe chronic kidney disease are potentially at risk of hyperkalemia (high potassium levels). This is because the kidneys cannot remove excess potassium from the blood. High potassium levels may cause life-threatening cardiac arrhythmias, muscle weakness, or paralysis.
People with kidney disease produce less erythropoietin (EPO), a hormone that signals to your bone marrow (spongy tissue inside most bones) to make red blood cells. With less EPO, your body makes fewer red blood cells, and as a result less oxygen is delivered to your organs and tissues.
People with chronic kidney disease also have more risk for heart problems. When the kidneys are not working effectively, it also changes the way the body handles cholesterol and other lipids, resulting inhigh cholesterol levels.
How is chronic kidney disease diagnosed?
Accurate diagnosis of CKD involves a combination of family history, laboratory tests, imaging studies, and renal biopsy when necessary. This section explores the diagnostic methods used to assess kidney function, including measurements of serum creatinine, eGFR, urine tests, and imaging studies.
Laboratory Tests
Blood tests, including serum creatinine, blood urea nitrogen (BUN), and other markers such as albumin are used for screening patients for kidney damage. Albumin is the most common type of protein in the urine. All patients with CKD should be screened for albuminuria. Persistent increased protein in the urine (two positive tests over 3 or more months) is the principal marker of kidney damage, acting as an early and sensitive marker in many types of kidney disease.
Urine Tests
Urine studies may show proteinuria (or albuminuria) and/or abnormalities in red or white blood cells on urine microscopy.
Imaging Studies
Imaging techniques, such as ultrasound, CT scan, and MRI, can provide valuable information about the structure and integrity of the kidneys.
Renal/Kidney Biopsy
In certain cases, a renal biopsy may be necessary to determine the underlying cause of kidney disease and guide treatment decisions.
What are the treatment options for chronic kidney disease?
The management of CKD aims to slow disease progression, manage complications, and improve the quality of life. This section explores the various treatment modalities employed in CKD management, including medications, dietary and fluid management, blood pressure control, anemia management, dialysis, and kidney transplantation.
Medications
Medications play a vital role in controlling blood pressure, managing complications, and slowing disease progression. This subsection discusses the pharmacological options, such as angiotensin-converting enzyme inhibitors (ACE inhibitors), angiotensin receptor blockers (ARBs), diuretics, and erythropoiesis-stimulating agents (ESAs), commonly used in CKD management.
Dietary and fluid management
Dietary and fluid management strategies are essential in CKD to maintain optimal nutritional status, manage fluid balance, and minimize the accumulation of waste products. This subsection explores dietary modifications, including sodium and protein restriction, and the importance of adequate fluid intake.
Blood Pressure control
Controlling blood pressure is crucial in slowing the progression of CKD and reducing the risk of cardiovascular complications. This subsection discusses target blood pressure goals and the use of antihypertensive medications in CKD management.
Anemia management
Anemia is a common complication of CKD, and its management involves addressing underlying causes and administering ESAs and iron supplementation when necessary. This subsection explores the management of anemia in CKD.
Dialysis
Dialysis is a life-sustaining treatment option for individuals with end-stage renal disease (ESRD). This subsection discusses the different types of dialysis, including hemodialysis and peritoneal dialysis, and their implications for CKD patients.
Kidney transplantation
Kidney transplantation is considered the best treatment option for eligible individuals with ESRD. This subsection explores the transplantation process, including donor selection, surgical procedure, and post-transplant care.
What are the strategies for managing chronic kidney disease?
Beyond medical interventions, effective CKD management requires a comprehensive approach that includes lifestyle modifications, patient education, multidisciplinary care, and supportive and palliative care. This section explores these management strategies and their impact on disease progression and overall well-being.
Lifestyle modifications
Lifestyle modifications, such as smoking cessation, regular physical activity, weight management, and avoidance of nephrotoxic substances, play a crucial role in slowing disease progression and improving outcomes. This subsection discusses the importance of lifestyle modifications in CKD management.
Patient education and self-management
Empowering individuals with CKD through patient education and self-management strategies enhances their ability to actively participate in their care. This subsection explores the importance of patient education, self-monitoring, medication adherence, and symptom management.
Multidisciplinary care
CKD management often involves a multidisciplinary healthcare team, including nephrologists, nurses, dietitians, social workers, and pharmacists. This subsection highlights the significance of collaborative care and care coordination in optimizing outcomes.
Supportive care and palliative care
Supportive care and palliative care are integral components of CKD management, particularly in the advanced stages of the disease. This subsection discusses the role of supportive care in managing symptoms, improving quality of life, and addressing end-of-life care.
What are the complications and co-morbidities of chronic kidney disease?
CKD is associated with a range of complications and co-morbidities that require close monitoring and management. This section explores cardiovascular, bone, and mineral disorders, anemia, malnutrition, and mental health issues commonly associated with CKD.
Cardiovascular disease
CKD significantly increases the risk of cardiovascular complications, such as hypertension, coronary artery disease, heart failure, and stroke. CKD means the kidneys don’t work well and this applies stress to the heart because the heart needs to pump harder to get blood to the kidneys. This can lead to heart disease, the leading cause of death in the United States.
Bone and mineral disorders
CKD disrupts mineral and bone metabolism, leading to bone loss, vascular calcification, and increased fracture risk. This subsection discusses the pathophysiology of bone and mineral disorders in CKD and the management strategies, including phosphate binders and vitamin D supplementation.
Anemia and iron deficiency
Anemia is a common complication of CKD and is primarily due to impaired production of erythropoietin. This subsection explores the causes, consequences, and management of anemia and iron deficiency in CKD.
Malnutrition
Malnutrition is prevalent in CKD and contributes to poor outcomes and reduced quality of life.
This subsection discusses the impact of CKD on nutritional status, the importance of nutritional assessment, and dietary interventions.
Depression and cognitive impairment
CKD is associated with an increased risk of mental health disorders, including depression and cognitive impairment. This subsection explores the psychological and cognitive consequences of CKD and the importance of addressing mental health needs in CKD patients.
How can chronic kidney disease be prevented or detected earlier?
Preventative strategies and early detection play a crucial role in reducing the burden of CKD. This section highlights the importance of managing risk factors, implementing screening programs, and promoting public health initiatives to prevent CKD and identify cases at an early stage.
Management of risk factors
Effective management of risk factors, such as diabetes, hypertension, and obesity, can prevent or delay the onset of CKD. This subsection discusses the strategies for managing modifiable risk factors and promoting a healthy lifestyle.
Screening and early diagnosis
Early detection of CKD through regular screenings, including blood and urine tests, is essential for timely intervention and disease management. This subsection explores the screening guidelines, the role of primary care providers, and the challenges in implementing screening programs.
Public health initiatives
Public health initiatives play a critical role in raising awareness, promoting healthy behaviors, and improving access to care for individuals at risk of CKD. This subsection discusses the importance of public health campaigns, policies, and community interventions in the prevention and early detection of CKD.
What chronic kidney disease support organizations are there available to support me in the UK?
- Kidney Care UK: Kidney Care UK is a national charity that supports individuals with kidney disease, including CKD. They offer information resources, educational materials, a helpline, support groups, and financial assistance programs.
- British Kidney Patient Association (BKPA): The BKPA is a charity organization that provides support and advocacy for kidney patients, including those with CKD. They offer resources, educational materials, a helpline, support groups, and financial assistance programs.
- National Kidney Federation (NKF): The NKF is a national charity that supports kidney patients, including those with CKD. They provide information resources, educational materials, a helpline, and support networks to help individuals manage their condition.
- Renal Association: The Renal Association is a professional body representing nephrologists and healthcare professionals involved in the care of kidney patients. While primarily focused on healthcare professionals, their website provides resources and information that can be helpful for individuals with CKD.
- Age UK: Age UK is a national charity that supports older people and provides information and resources on various health conditions, including CKD. They offer advice, educational materials, and support services that can assist individuals in understanding and managing their condition.
What chronic kidney disease support organizations are there available to support me in the US?
- National Kidney Foundation (NKF): The National Kidney Foundation is a leading organization dedicated to the awareness, prevention, and treatment of kidney diseases, including CKD. They offer educational resources, support services, advocacy initiatives, community events, and a helpline.
- American Association of Kidney Patients (AAKP): The AAKP is a national non-profit organization that advocates for kidney patients and provides resources, education, and support to individuals living with CKD. They offer patient education materials, a helpline, advocacy initiatives, and a patient engagement network.
- American Kidney Fund (AKF): The AKF is a non-profit organization that provides financial assistance, education, and support services to individuals with kidney disease, including CKD. They offer grants, resources, educational materials, advocacy initiatives, and a helpline.
- Renal Support Network (RSN): The RSN is a non-profit, patient-led organization that provides support and empowerment to individuals with CKD. They offer educational resources, peer support, advocacy initiatives, and a telephone support line.
- National Kidney Disease Education Program (NKDEP): The NKDEP is an initiative of the National Institutes of Health (NIH) that aims to raise awareness and provide resources on kidney health and CKD prevention. They offer educational materials, resources for healthcare professionals, and tools for individuals to understand and manage their kidney health.
Summary
Chronic kidney disease is a significant public health concern, affecting millions of individuals worldwide. This comprehensive essay has provided a detailed exploration of CKD, including its definition, etiology, risk factors, pathophysiology, clinical manifestations, diagnosis, treatment modalities, management strategies, and preventive measures. By understanding the complexities of CKD and implementing appropriate interventions, healthcare professionals and individuals with CKD can work together to slow disease progression, manage complications, and improve the overall quality of life for those affected by this condition. Continued research, education, and advocacy are vital in addressing the global burden of CKD and improving outcomes for individuals with this chronic condition.
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.