Menopause
Get valuable insights into Menopause, including its causes, symptoms, prevention strategies, and treatment options, while also learning about how you can lower the cost of the medications used to treat Menopause.

MEDICAL INFORMATION
Menopause Key Facts
Related Medications
Natural Menopause is a phase in a woman’s life that marks the end of her reproductive years. It typically occurs in midlife. Here, we aim to provide you with a thorough understanding of menopause, including its definition, hormonal changes, common symptoms, health implications, and management options. By exploring the intricacies of menopause, individuals and healthcare professionals can gain valuable insights into this significant life transition and develop personalised approaches to promote women’s health and well-being.
What is the definition of menopause?
Menopause is defined as the permanent cessation of menstruation and the end of a woman’s reproductive years. It marks the natural transition in a woman’s life when the ovaries gradually stop producing eggs, resulting in a decline in reproductive hormones, particularly oestrogen and progesterone. Menopause is officially diagnosed after a woman has gone 12 consecutive months without a menstrual period.
Women typically experience menopause between the ages of 45 and 55, but the exact timing can vary for each individual. Menopause between the ages of 40 and 45 is called early menopause. However in a very small number of people, roughly 1% of women, menopause can happen before the age of 40. This is called premature menopause. The process leading up to menopause is called perimenopause, during which hormone levels fluctuate, menstrual cycles may become irregular, and menopausal symptoms may manifest. Post-menopause refers to the period following menopause when the body has fully adjusted to the absence of menstrual cycles.
Women who have a hysterectomy procedure where the ovaries are removed, will experience menopause immediately, regardless of age. This is called surgical menopause.
Menopause is a natural part of the aging process and signals the end of a woman’s fertility. While it is a physiological change, menopause can also have significant physical and emotional effects on women’s health and well-being. Understanding the definition and implications of menopause can empower women to navigate this life stage with knowledge and seek appropriate care and support.
What hormonal changes happen during menopause?
During menopause, hormonal changes occur as the ovaries gradually decrease their production of reproductive hormones, particularly oestrogen and progesterone. These hormonal changes play a significant role in the physical and physiological changes that accompany menopause. Here are the key hormonal changes that happen during menopause
Decline in Estrogen Levels
- Estrogen, primarily produced by the ovaries, is responsible for regulating the menstrual cycle and maintaining various aspects of female reproductive health
- During menopause, estrogen levels decrease significantly, leading to irregular menstrual cycles and eventually the cessation of menstruation
- Estrogen decline is associated with various symptoms such as hot flashes, night sweats, vaginal dryness, and changes in bone density
Decline in Progesterone Levels
- Progesterone, also produced by the ovaries, is involved in preparing the uterus for pregnancy and supporting early pregnancy
- As menopause approaches, progesterone levels decrease, leading to changes in menstrual patterns and eventually the absence of ovulation
- Lower progesterone levels can contribute to symptoms such as irregular bleeding, mood swings, and changes in sleep patterns
Increase in Follicle-Stimulating Hormone (FSH) Levels
- Follicle-Stimulating Hormone (FSH) is produced by the pituitary gland and plays a role in stimulating the growth and development of ovarian follicles
- As the ovaries produce less estrogen, the feedback mechanism between the ovaries and pituitary gland is disrupted, resulting in increased FSH levels
- Elevated FSH levels are commonly observed during menopause and can contribute to menopausal symptoms such as hot flashes and night sweats
Changes in Other Hormones
- Other hormones, such as testosterone and dehydroepiandrosterone (DHEA), may also decrease during menopause
- Testosterone, although primarily associated with male reproductive health, is important for women as well and contributes to libido, muscle mass, and overall well-being
- Decreased testosterone levels during menopause can result in reduced sexual desire and changes in body composition
- DHEA, an adrenal hormone, may decline with age and can affect energy levels and overall vitality
It’s important to note that the hormonal changes during menopause are complex and can vary among individuals. The timing and extent of these changes can influence the severity and duration of menopausal symptoms experienced by each woman
What are the symptoms of menopause?
Menopause is a natural biological process that involves hormonal changes, and it can be accompanied by a range of symptoms. It’s important to note that the severity and duration of symptoms can vary among individuals. Here are some common symptoms experienced during menopause:
Irregular Menstrual Cycles
Menstrual periods may become irregular in terms of timing, flow, or duration during the perimenopausal phase before menopause. Eventually, menstruation ceases altogether.
Hot Flashes and Night Sweats (Vasomotor Symptoms)
Sudden feelings of intense heat, typically accompanied by sweating and flushing of the face, neck, and chest. Night sweats refer to hot flashes that occur during sleep and may disrupt sleep patterns.
Vaginal and Urinary Changes
- Vaginal Dryness: Reduced estrogen levels can lead to vaginal dryness, itching, discomfort during intercourse, and an increased risk of vaginal infections
- Urinary Symptoms: Some women experience changes in urinary frequency, urgency, or recurrent urinary tract infections due to the impact of estrogen decline on the genitourinary tissues
Sleep Disturbances
Menopause-related symptoms, such as hot flashes, night sweats, or anxiety, can disrupt sleep patterns and contribute to insomnia or overall poor sleep quality.
Mood Changes
Fluctuating hormone levels can contribute to mood swings, irritability, anxiety, or feelings of sadness or depression in some women.
Changes in Sexual Function
Reduced estrogen levels can affect sexual desire, arousal, and vaginal lubrication, potentially leading to a decreased interest in sexual activity or discomfort during intercourse.
Physical Changes
- Changes in Breast Tissue: Some women may experience changes in breast size, fullness, or tenderness
- Weight Gain: Hormonal changes and aging metabolism can lead to weight gain or a shift in body fat distribution, particularly around the abdomen
- Muscle and Joint Discomfort: Some women may experience muscle aches, joint pain, or increased stiffness
Cognitive Changes
Some women report difficulties with memory, concentration, or “brain fog” during menopause, although the impact on cognitive function is still an area of ongoing research.
It’s important to remember that not all women experience every symptom, and individual experiences may vary. If menopausal symptoms significantly affect quality of life or daily functioning, it is recommended to consult with a healthcare professional for appropriate guidance, management strategies, and potential treatment options.
What are the long term risks and complications of menopause?
Menopause itself is a natural process and not considered a disease. However, the hormonal changes and aging process associated with menopause can have long-term health implications. It’s important to note that individual experiences and risks may vary. Here are some potential long-term risks associated with menopause
Osteoporosis
The decline in estrogen levels during menopause can contribute to bone loss and increase the risk of osteoporosis, a condition characterized by weak and brittle bones. Women post-menopause are at an increased risk of fractures, particularly in the hips, spine, and wrists.
Cardiovascular Disease
Estrogen has a protective effect on the cardiovascular system, and its decline during menopause may increase the risk of medical conditions like heart disease and stroke. Other risk factors like age, family history, lifestyle choices, and underlying conditions can further contribute to cardiovascular risks.
Changes in Cholesterol Levels
Menopause can lead to unfavorable changes in lipid profiles, such as increased total cholesterol levels, decreased levels of high-density lipoprotein (HDL) cholesterol (known as “good” cholesterol), and increased levels of low-density lipoprotein (LDL) cholesterol (known as “bad” cholesterol). These changes may contribute to an increased risk of cardiovascular disease.
Genitourinary Health Issues
The decline in estrogen levels can impact the health of the urinary and genital tissues, leading to issues such as urinary incontinence, recurrent urinary tract infections, and vaginal dryness. These changes can affect urinary and sexual function and impact quality of life.
- Cognitive Health: Some research suggests that the decline in estrogen levels during menopause may be associated with a small increased risk of cognitive decline and dementia. However, the relationship between menopause and cognitive health is complex and still an area of ongoing research
- Metabolic Changes: Hormonal changes during menopause can affect metabolism and contribute to weight gain, particularly around the abdominal area. This can increase the risk of metabolic conditions like insulin resistance, type 2 diabetes, and metabolic syndrome
- Breast cancer: There is an higher risk of developing breast and endometrial cancer if menopause starts after the age of 55
It’s important to note that while these risks may be associated with menopause, they can also be influenced by other factors such as age, lifestyle choices, genetic predisposition, and pre-existing health conditions. Managing these risks involves adopting a healthy lifestyle, regular health screenings, maintaining a balanced diet, engaging in regular physical activity, managing weight, and working closely with healthcare professionals to monitor and address specific health concerns.
How is menopause diagnosed?
Menopause is a natural biological process that marks the end of a woman’s menstrual cycles and fertility, usually diagnosed retrospectively after a woman has missed her periods for 12 consecutive months (assuming that there is no other obvious medical cause). It typically occurs in women with an average age between 45 and 55.
While there’s no specific test to definitively diagnose menopause, the following approaches can help indicate if a woman is in the perimenopausal stage (the transition period leading up to menopause) or has indeed reached menopause:
Medical History and Physical Examination
The healthcare provider will usually start by asking about menstrual history, changes in menstrual cycles, and symptoms such as hot flashes, sleep disturbances, mood changes, and sexual issues.
Blood Tests
While not always necessary, a healthcare provider may recommend blood tests to measure the levels of certain hormones, such as:
- Follicle-stimulating hormone (FSH): FSH levels tend to increase as a woman reaches menopause because the ovaries aren’t responding as well to the FSH, so the brain produces more
- Estradiol: As a woman approaches menopause, her levels of this form of estrogen decrease
Other tests
Other tests may be done to rule out other conditions that could be causing symptoms similar to those of menopause, such as thyroid disease.
While tests can help in the diagnosis, the most significant factor in diagnosing menopause is the absence of menstruation for one full year. It’s important to have regular check-ups with a healthcare provider during this period to manage any symptoms and monitor for conditions that are more common after menopause, like osteoporosis and heart disease.
What are the treatment options for menopause?
There are several treatment options available to manage the symptoms and improve the quality of life during menopause. The choice of treatment depends on the severity of symptoms, overall health, personal preferences, and individualised discussions with healthcare professionals. Here are common treatment options for menopause
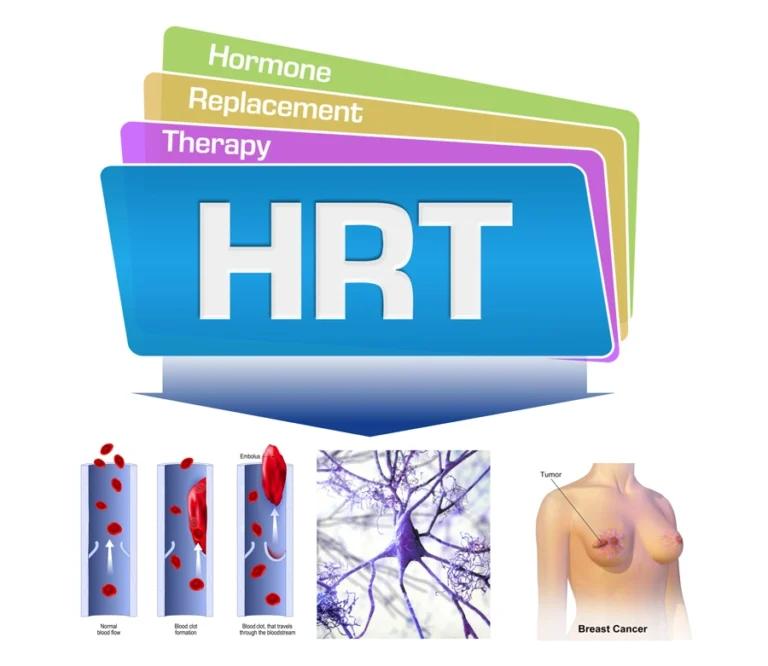
Hormone Therapy (HT)
- Estrogen Therapy: Systemic estrogen in the form of pills, patches, gels, creams, or sprays can be prescribed to relieve symptoms like hot flashes, vaginal dryness, and night sweats. It’s usually recommended at the lowest effective dose for the shortest duration needed
- Estrogen-Progestin Therapy: Women with an intact uterus are generally prescribed a combination of estrogen and progestin to reduce the risk of endometrial cancer. This is important as estrogen alone can increase the risk of endometrial cancer in women with a uterus
Non-Hormonal FDA and MHRA approved Medications
- Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): These antidepressant medications can help manage hot flashes and mood-related symptoms
- Gabapentin and Pregabalin: These anticonvulsant medications may be prescribed to reduce hot flashes and other menopausal symptoms
- Clonidine: Originally used to treat high blood pressure, clonidine can also be prescribed off-label to manage hot flashes
- Low-dose estrogen in the form of vaginal creams, tablets, or rings can be used to relieve vaginal dryness, discomfort during intercourse, and urinary symptoms. Vaginal estrogen delivers a localized effect and is generally considered safe for most women
Lifestyle Changes
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can help manage weight, support overall health, and alleviate symptoms
- Regular Exercise: Engaging in regular physical activity, such as aerobic exercise and strength training, can help manage weight, improve mood, promote bone health, and reduce the severity of hot flashes
- Stress Reduction Techniques: Stress management techniques like relaxation exercises, deep breathing, meditation, and yoga can help alleviate symptoms and improve overall well-being
- Adequate Sleep: Implementing good sleep hygiene practices and creating a conducive sleep environment can help manage sleep disturbances during menopause
Supplements and Complementary therapy
- Black Cohosh
- Soy Isoflavones
What medications are used to treat the symptoms of menopause?
There are several medications commonly used to treat symptoms associated with menopause. These medications can help alleviate specific symptoms and improve overall quality of life. Here are some medications used in the treatment of menopause
Estrogen/Progestin
– Estrogen Therapy: Estrogen can be administered in various forms, including pills, patches, gels, creams, or sprays. It is effective in relieving symptoms such as hot flashes, night sweats, and vaginal dryness. Estrogen therapy is generally prescribed at the lowest effective dose for the shortest duration needed.
– Estrogen-Progestin Therapy: Women with an intact uterus are typically prescribed a combination of estrogen and progestin to reduce the risk of endometrial cancer. Progestin is added to counteract the potential stimulation of the uterine lining by estrogen.
Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
These antidepressant medications, such as fluoxetine, paroxetine, venlafaxine, and desvenlafaxine, can effectively manage hot flashes, night sweats, and mood-related symptoms associated with menopause. They work by regulating the neurotransmitters serotonin and norepinephrine.
Gabapentin and Pregabalin
These anticonvulsant medications can help reduce the frequency and severity of hot flashes. Gabapentin and pregabalin are particularly useful for women who cannot take hormone therapy or prefer non-hormonal options.
Clonidine
Originally used to treat high blood pressure, clonidine is sometimes prescribed off-label to manage hot flashes. It can be beneficial for women who cannot take hormone therapy or other medications.
Vaginal Estrogen
Low-dose estrogen in the form of creams, tablets, or rings can be applied locally to the vagina to alleviate symptoms of vaginal dryness (atrophy), discomfort during intercourse, and urinary symptoms. Vaginal estrogen delivers a localized effect and is generally considered safe for most women.
Calcium
Post menopausal women are encouraged to supplement with Calcium due to reduced calcium absorption.
Moisturizers
Vaginal moisturisers such as K-Y, Replens, among others, are used every few days to help maintain healthy vaginal tissues by providing necessary moisture.
What support is available to women going through menopause in the UK?
In the UK, there are various sources of support and resources available to women going through menopause. These organisations and initiatives aim to provide information, guidance, and a supportive community for women navigating the menopausal transition. Here are some examples of support available in the UK:
- Women’s Health Concern (WHC): WHC is the patient arm of the British Menopause Society (BMS), providing a range of resources about menopause and women’s health
- The British Menopause Society (BMS): BMS provides education, information and guidance to healthcare professionals specialising in all aspects of post reproductive health
- Menopause Matters: An independent website providing up-to-date, accurate information about the menopause, menopausal symptoms and treatment options
- NHS: The National Health Service offers a comprehensive guide to menopause, including symptoms, diagnosis, treatment, and self-help tips
- The Daisy Network: A support group for women who experience a premature menopause. They provide a support network of meetings and an informative website
- Menopause Support: A not for profit community interest organisation offering advice and support to women
What support is available to women going through menopause in the US?
In the United States, there are several sources of support and resources available to women going through menopause. These organisations and initiatives aim to provide information, guidance, and a supportive community for women navigating the menopausal transition. Here are some examples of support available in the US
- The North American Menopause Society (NAMS): NAMS provides resources and support for women to gain an understanding of menopause
- American Menopause Foundation (AMF): AMF offers educational materials about menopause and promotes research on menopause-related issues
- Women’s Health (Office on Women’s Health, U.S. Department of Health and Human Services): This government website provides reliable, accurate, commercial free information on a variety of women’s health topics, including menopause
- Red Hot Mamas: This is a national menopause education program providing mid-life women’s health information and support which also offers community-based, free education programs
- National Institute on Aging: Part of the National Institutes of Health, this institute offers comprehensive information on a wide range of aging-related topics, including menopause
Summary
Menopause is a natural biological process that represents a significant life transition for women. By understanding its hormonal changes, common symptoms, health implications, and management options, women can navigate this phase with knowledge and confidence. Open communication with healthcare professionals and a holistic approach to menopause management can help women maintain their overall health and well-being during this transformative time.
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.