Schizophrenia
Get valuable insights into Schizophrenia, including its causes, symptoms, prevention strategies, and treatment options, while also learning about how you can lower the cost of the medications used to treat Schizophrenia.

MEDICAL INFORMATION
Schizophrenia Key Facts
Related Medications
Schizophrenia is a complex and chronic mental health disorder that affects millions of people worldwide. It is a serious mental illness that affects the way a person feels, behaves and thinks. Here we aim to provide you with a comprehensive overview of schizophrenia, including its definition, symptoms, causes, risk factors, and available treatment options. By understanding the complexities of this disorder, individuals, families, and healthcare professionals can promote early detection, appropriate interventions, and improved quality of life for individuals living with schizophrenia.
What is the definition of schizophrenia?
Schizophrenia is a chronic and severe psychotic disorder that affects the way a person thinks, feels, and behaves. It is characterized by a combination of symptoms that can include hallucinations, delusions, disorganized thinking and speech, social withdrawal, reduced emotional expression, and difficulties in cognitive functioning. Schizophrenia impacts a person’s ability to perceive reality accurately, often resulting in significant impairments in daily functioning and relationships.
The symptoms of schizophrenia are divided into two main categories: positive symptoms and negative symptoms. Positive symptoms involve the presence of abnormal experiences or behaviors that are not typically seen in healthy individuals, such as hallucinations (perceiving things that are not there) and delusions (holding false beliefs). Negative symptoms refer to a loss or reduction of normal functions, including reduced emotional expression, social withdrawal, and cognitive difficulties.
Schizophrenia is a complex disorder with a varied course and presentation. It affects each individual differently, and the severity of symptoms can fluctuate over time. The onset of schizophrenia typically occurs in late adolescence or early adulthood, and it is considered a lifelong condition. However, with early detection, appropriate treatment, and ongoing support, individuals with schizophrenia can achieve symptom management and improved quality of life.
Is schizophrenia a personality disorder?
No. Schizophrenia is not a personality disorder.
What are the symptoms of schizophrenia?
Schizophrenia is a complex mental health disorder that can present a range of symptoms. These symptoms can vary in intensity and may change over time. Here are the main symptoms of schizophrenia
Positive symptoms
- Hallucinations: Sensory experiences that are not based on real stimuli, most commonly auditory hallucinations (hearing voices), but can also involve visual, olfactory, tactile, or gustatory sensations
- Delusions: False beliefs that are firmly held despite evidence to the contrary. Delusions can involve various themes, such as paranoia (believing one is being targeted or persecuted), grandiosity (believing one has exceptional abilities or importance), or religious or somatic delusions
- Disorganized thinking and speech: Incoherent or illogical thinking, difficulty organizing thoughts, and tangential or irrelevant speech patterns
Negative symptoms
- Reduced emotional expression: Decreased display of emotions through facial expressions, tone of voice, or body language
- Avolition: decreased motivation, lack of interest or initiative, and difficulty in setting and achieving goals
- Anhedonia: Reduced ability to experience pleasure or enjoyment
- Social withdrawal: Decreased desire to engage in social interactions, leading to isolation and reduced social functioning
- Cognitive impairment: Difficulties in attention, memory, decision-making, and problem-solving
Cognitive symptoms
- Impaired working memory: Difficulties in holding and manipulating information in the mind
- Attention deficits: Trouble sustaining attention or focusing on specific tasks
- Executive functioning problems: Challenges in planning, organizing, and executing tasks
It’s important to note that not all individuals with schizophrenia experience all of these symptoms, and the severity and combination of symptoms can vary. Additionally, the presence of these symptoms alone does not necessarily indicate schizophrenia, as other conditions or factors can cause similar symptoms. A comprehensive evaluation by a healthcare professional is necessary for an accurate diagnosis and appropriate treatment.
What are the types and sub-types of schizophrenia?
Schizophrenia is a complex mental health disorder that can be categorized into different types and subtypes based on the predominant symptoms and clinical presentation. The classification of subtypes may vary depending on the diagnostic criteria used. Here are the main types and subtypes of schizophrenia:
Paranoid schizophrenia
This subtype is characterized by prominent delusions and auditory hallucinations related to persecution or grandiosity. Individuals with paranoid schizophrenia may exhibit heightened suspicions, paranoia, and a preoccupation with these delusions, often with intact cognitive functioning
Disorganized schizophrenia (formerly known as Hebephrenic Schizophrenia)
Disorganized schizophrenia is characterized by disorganized thinking, speech, and behavior. Individuals may exhibit inappropriate emotional responses, difficulty organizing their thoughts, and their speech may be incoherent or tangential. Daily functioning is often significantly impaired
Catatonic schizophrenia
Catatonic schizophrenia is characterized by extreme disturbances in motor behavior. Individuals may exhibit either excessive, purposeless movements or extreme physical immobility. Other symptoms can include mutism, echolalia (repeating others’ words), or echopraxia (imitating others’ actions)
Undifferentiated schizophrenia
This subtype is diagnosed when symptoms do not clearly fit into one of the specific subtypes mentioned above. It represents a mixed or generalized presentation of schizophrenia
Residual schizophrenia
Residual schizophrenia occurs when an individual no longer experiences prominent positive symptoms (e.g., hallucinations or delusions) but may still exhibit mild residual symptoms or negative symptoms. These residual symptoms may include reduced emotional expression, social withdrawal, or cognitive difficulties
It’s important to note that the classification of subtypes is not always definitive, and individuals with schizophrenia may exhibit a combination of symptoms from different subtypes. Furthermore, the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) no longer recognizes subtypes as formal diagnostic categories but acknowledges that clinicians may still find them useful for descriptive purposes.
Also, it is important to recognize that mental health conditions can be mistaken for each other. For example, While bipolar disorder and schizophrenia are both chronic in nature and have some overlapping symptoms, they are distinct mental health conditions. Bipolar disorder is primarily characterized by severe shifts in mood, while the predominant features of schizophrenia are hallucinations and delusions.
Another example is schizoaffective disorder. Understanding the distinctions between schizoaffective disorder and schizophrenia can be challenging, given that both disorders encompass central psychotic symptoms such as hallucinations, delusions, and disorganized thought. However, they are separate conditions, each characterized by its own specific diagnostic criteria and therapeutic approaches.
A comprehensive evaluation by a healthcare professional is necessary to determine the specific subtype and develop an appropriate treatment plan.
What are the causes and risk factors associated with schizophrenia?
The exact cause of schizophrenia is not yet fully understood. However, research suggests that a combination of genetic, environmental, and neurobiological factors contribute to the development of the disorder. Here are the main causes and risk factors associated with schizophrenia:
Genetic Factors
- Family history: Having a close family member (such as a parent or sibling) with schizophrenia increases the risk of developing the disorder
- Genetic Variations: Certain genetic variations or mutations may influence the vulnerability to schizophrenia. However, no single gene is solely responsible, and the interaction of multiple genes is likely involved
Neurochemical and neurodevelopmental factors
- Dopamine imbalance: Dysfunction in the dopamine neurotransmitter system, specifically an overactivity of dopamine, is believed to play a role in schizophrenia
- Abnormal brain structure and Function: Differences in brain structure, including enlarged ventricles and reduced gray matter volume, have been observed in individuals with schizophrenia. Neurodevelopmental abnormalities during early brain development may contribute to these structural differences
Environmental factors
- Prenatal and Birth Complications: Exposure to infections during pregnancy, maternal malnutrition, maternal stress, obstetric complications (e.g., prolonged labor, low birth weight), and complications during childbirth may increase the risk of schizophrenia
- Substance use: Drug use, such as cannabis, especially during adolescence or in individuals already at risk, may contribute to the development of schizophrenia
- Urban environment: Growing up in urban areas or living in densely populated areas may be associated with a higher risk of schizophrenia, possibly due to increased stress, social adversity, or exposure to environmental toxins
Other risk factors
- Gender: Men tend to develop schizophrenia at an earlier age than women and have a slightly higher overall risk
- Age: The risk of developing schizophrenia is highest in late adolescence and early adulthood
- Family dynamics and socioeconomic Factors: Adverse family environments, childhood trauma, social isolation, and low socioeconomic status may contribute to the risk of schizophrenia
It’s important to note that having one or more risk factors does not guarantee the development of schizophrenia. Many individuals with risk factors do not develop the disorder, while some without obvious risk factors can still develop schizophrenia. The interplay between genetic predisposition and environmental factors likely contributes to the complex nature of the disorder.
What is the pathophysiology of schizophrenia?
The pathophysiology of schizophrenia, the underlying biological processes involved in the development and manifestation of the disorder, is complex and not fully understood. However, research suggests that multiple factors contribute to the pathophysiology of schizophrenia. Here are some key aspects
Neurotransmitter imbalance:
- Dopamine hypothesis: One of the prominent theories suggests that abnormalities in the dopamine neurotransmitter system play a significant role in schizophrenia. It is believed that an overactivity of dopamine in certain brain regions, particularly the mesolimbic pathway, contributes to positive symptoms like hallucinations and delusions
- Glutamate hypothesis: Dysfunction in the glutamate neurotransmitter system, specifically the N-methyl-D-aspartate (NMDA) receptor, has also been implicated. Reduced glutamate activity may lead to impaired neural connectivity and contribute to cognitive and negative symptoms
Neurodevelopment abnormalities
- Disrupted brain development: Schizophrenia is thought to involve neurodevelopmental abnormalities, likely occurring during prenatal and early childhood periods. These abnormalities may affect neural circuits, brain structure, and connectivity
- Abnormal synaptic pruning: During adolescence, there is a normal process of synaptic pruning, where unnecessary connections in the brain are eliminated. In individuals with schizophrenia, this process may be altered, leading to abnormal synaptic connectivity and disrupted neural communication
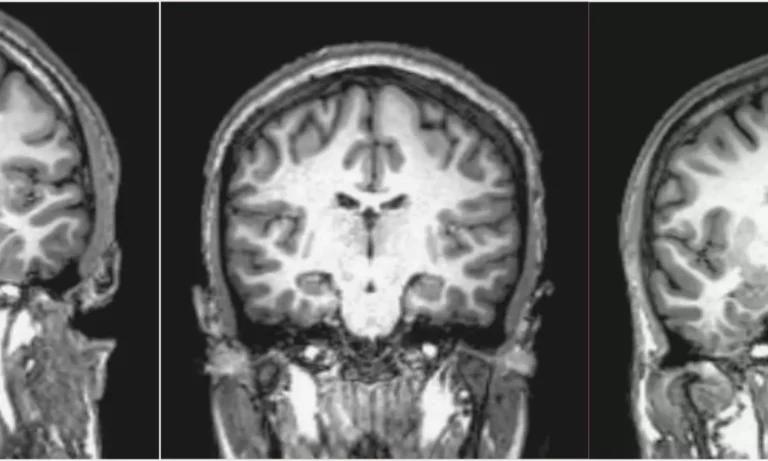
Structural and functional brain abnormalities
- Reduced gray matter volume: Studies have shown that individuals with schizophrenia may exhibit reduced gray matter volume in certain brain regions, including the prefrontal cortex, hippocampus, and temporal lobes
- Enlarged ventricles: Increased ventricular size, indicating reduced brain tissue volume, has been observed in people with schizophrenia
- Altered connectivity: Disruptions in functional connectivity, or the coordination of activity between different brain regions, have been observed, suggesting a breakdown in the integration of neural networks
Genetic and environmental factors
- Genetic predisposition: Genetic factors contribute to the susceptibility to schizophrenia. Several genes have been implicated, but there is no single gene solely responsible for the disorder. Rather, it is likely a combination of genetic variations and interactions
- Environmental influences: Environmental factors, such as prenatal infections, complications during pregnancy or birth, and exposure to stressors, may interact with genetic vulnerabilities and contribute to the development of schizophrenia
It’s important to note that the pathophysiology of schizophrenia is multifactorial, involving complex interactions between genetic, neurochemical, and environmental factors.
How is schizophrenia diagnosed?
In most people with schizophrenia, symptoms commonly surface around the mid to late 20s, though it can start later, up to the early 30s. Schizophrenia is typically diagnosed by a psychiatrist, clinical psychologist or mental health professional through a combination of a thorough clinical interview, observation, and sometimes additional diagnostic tests. Here are the common steps used in diagnosing schizophrenia:
Medical history and physical examination
A healthcare provider will start by asking about personal and family medical history. They may also conduct a physical examination to rule out physical illnesses that could be causing psychotic symptoms
Psychiatric evaluation
This involves discussing thoughts, feelings, and behavior patterns. The patient may also be asked about thoughts of suicide, self-harm, or harm to others. The provider will assess the person’s appearance, demeanor, and ability to think, reason, and express themselves
Diagnostic criteria
The diagnosis of schizophrenia is based on the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association. The DSM-5 criteria for schizophrenia include two or more of the following symptoms present for a significant portion of time during a one-month period: delusions, hallucinations, disorganized speech, disorganized or catatonic behavior, negative symptoms (such as diminished emotional expression or avolition)
Duration of symptoms
According to the DSM-5, for a diagnosis of schizophrenia, some level of disturbance must last for at least six months. This period must include at least one month of active-phase symptoms (two if hallucinations and delusions are not among them)
Exclusion of other disorders
It’s important to rule out other mental health disorders that may have similar symptoms, such as bipolar disorder or depressive disorder with psychotic features. Substance abuse, certain medical conditions and medications can also cause symptoms similar to those of schizophrenia
Functional impairment
There is often significant impairment in one or more major areas of functioning such as work, interpersonal relations, or self-care
Neuroimaging or lab tests
While there are no laboratory or imaging tests that can independently diagnose schizophrenia, tests such as brain imaging or blood tests might be done to help rule out other conditions that have similar symptoms, such as a brain tumor, seizure disorder, or substance-induced psychosis
It’s important to note that diagnosing schizophrenia is a complex process that should be done by a qualified healthcare provider. Early diagnosis and treatment can improve the long-term outlook for people with schizophrenia.
What are the treatment approaches for schizophrenia?
The treatment of schizophrenia typically involves a comprehensive approach that combines medication, psychotherapy, psychosocial interventions, and support services.
Antipsychotic Medications
- Antipsychotic medications are the primary treatment for schizophrenia. They help manage the symptoms of psychosis, such as hallucinations, delusions, and disordered thinking
- First-generation (typical) antipsychotics, such as haloperidol and chlorpromazine, and second-generation (atypical) antipsychotics, such as risperidone and olanzapine, are commonly prescribed
- The choice of medication depends on factors such as the individual’s symptoms, response to treatment, side effect profile, and personal considerations
Psychotherapy
- Cognitive behavioral therapy (CBT): CBT can help individuals identify and modify unhelpful thoughts, beliefs, and behaviors associated with their symptoms. It focuses on managing distress, improving coping skills, and enhancing problem-solving abilities
- Family therapy: Involving family members in therapy can help improve communication, understanding, and support for the individual with schizophrenia. It can also address family dynamics and educate family members about the illness
- Supportive therapy: Supportive therapy provides emotional support, validation, and encouragement to individuals with schizophrenia, helping them cope with the challenges of the disorder
Psychosocial interventions
- Social skills training: Social skills training helps individuals improve their communication, interpersonal skills, and problem-solving abilities, promoting better social functioning and integration
- Vocational rehabilitation: Vocational programs assist individuals in developing employment skills, finding job opportunities, and maintaining employment
- Cognitive remediation: Cognitive remediation focuses on improving cognitive functioning, such as attention, memory, and problem-solving skills, through targeted training and exercises
- Assertive community treatment (ACT): ACT programs provide comprehensive community-based support, including case management, medication monitoring, and assistance with daily living skills
Hospitalization
- In severe cases or during acute psychotic episodes, short-term hospitalization may be necessary to ensure safety, stabilize symptoms, and adjust medications
- Partial hospitalization programs and intensive outpatient programs offer structured treatment and support while allowing individuals to reside in the community
Self-help and support
- Peer support: Engaging with support groups and peer networks can provide individuals with schizophrenia a sense of belonging, understanding, and shared experiences
- Education and psychoeducation: Learning about schizophrenia and its management through educational programs and psychoeducation sessions can empower individuals and their families to actively participate in their treatment and recovery
Electroconvulsive therapy (ECT)
- ECT, or electroconvulsive therapy, is a medical treatment that involves sending small electric currents through the brain to trigger a brief seizure. ECT can often rapidly reverse symptoms of certain mental health conditions, including severe depression, mania, and catatonia. It’s usually used as a last resort treatment when other treatments have failed, are too risky, or cannot be tolerated
In the context of schizophrenia, ECT is sometimes used to treat severe cases where medication and other therapies have been ineffective. It’s particularly useful for those with catatonic symptoms, or when the person with schizophrenia is also experiencing severe depression
Treatment for schizophrenia is often long-term and requires ongoing monitoring and adjustment. Collaborative care involving a multidisciplinary team of healthcare professionals, including psychiatrists, psychologists, social workers, and occupational therapists, is essential to provide holistic and comprehensive support. Early intervention, adherence to treatment, and regular follow-up care are crucial for managing symptoms, improving functioning, and promoting recovery in individuals with schizophrenia.
What medications are used to treat schizophrenia?
The treatment of schizophrenia typically involves the use of antipsychotic medications, which help manage the symptoms of psychosis associated with the disorder. There are two main categories of antipsychotic medications: first-generation (typical) antipsychotics and second-generation (atypical) antipsychotics. Here are some commonly prescribed medications for schizophrenia:
First-Generation antipsychotics
- Haloperidol (Haldol)
- Chlorpromazine (Thorazine)
- Fluphenazine (Prolixin)
- Perphenazine (Trilafon)
- Thioridazine (Mellaril)
Second-Generation Antipsychotics
- Risperidone (Risperdal)
- Olanzapine (Zyprexa)
- Quetiapine (Seroquel)
- Aripiprazole (Abilify)
- Ziprasidone (Geodon)
- paliperidone palmitate (Invega)
- Clozapine (Clozaril)
The choice of medication depends on various factors, including the individual’s symptoms, treatment response, side effect profile, medical history, and personal considerations. Second-generation antipsychotics are generally preferred due to their lower risk of movement disorders, such as extrapyramidal symptoms, compared to first-generation antipsychotics. Clozapine is often reserved for individuals who have not responded to other antipsychotic medications, as it has unique efficacy in treatment-resistant cases but requires regular monitoring due to the risk of agranulocytosis (a potentially serious blood condition).
The dosage and duration of medication treatment are determined by the individual’s response and ongoing assessment by a healthcare professional. It is important to note that medication alone is not always sufficient, and a comprehensive treatment approach involving psychotherapy, psychosocial interventions, and support services is generally recommended for managing schizophrenia effectively.
What support organizations are available for schizophrenia in the US?
In the United States, there are several organizations that provide support, resources, and advocacy for individuals with schizophrenia and their families. Here are a few:
- National Alliance on Mental Illness (NAMI): This is the largest grassroots mental health organization in the U.S. They offer a range of services, including a helpline, support groups, educational programs, and advocacy efforts
- Schizophrenia and Related Disorders Alliance of America (SARDAA): This organization provides resources and support specifically for individuals and loved ones with schizophrenia and related disorders. They also offer support groups, educational materials, and advocacy initiatives
- Brain & Behavior Research Foundation: This foundation funds scientific research to alleviate the suffering caused by mental illness, including schizophrenia. They also provide resources and information about mental health disorders
- Mental Health America (MHA): While not focused exclusively on schizophrenia, MHA provides resources, advocacy, and public education about all forms of mental illness
- Treatment Advocacy Center: This national nonprofit organization is dedicated to eliminating barriers to the timely and effective treatment of severe mental illnesses, including schizophrenia. The center promotes laws, policies, and practices for the delivery of psychiatric care
- American Psychiatric Association (APA): The APA provides resources and support for psychiatric professionals, but also offers a wealth of information and resources for patients and families, including the latest news and research on schizophrenia
- Schizophrenia – national institute of mental health
What support organizations are available for schizophrenia in the UK?
In the United Kingdom, several organizations provide support, resources, and advocacy for individuals with schizophrenia and their families. Here are a few:
- Rethink Mental Illness: This UK-based charity provides a wide range of services for people with mental health conditions, including schizophrenia. This includes advice and information, support groups, and advocacy services
- Mental Health Foundation: This charity focuses on prevention and understanding of mental health conditions. They have resources and information on schizophrenia
- SANE: This charity provides emotional support, guidance, and information to anyone affected by mental illness, including schizophrenia. They also operate a mental health helpline
- Mind: Mind provides advice and support for anyone facing a mental health problem. They campaign to improve services, raise awareness, and promote understanding
- National Schizophrenia Fellowship (NSF, Scotland): This Scotland-based organization is part of the larger UK group, Rethink Mental Illness. They provide support and resources for individuals with schizophrenia
- Together for Mental Wellbeing: This organization supports people through community services, including housing, criminal justice, and mental health advocacy
- Hearing Voices Network: While not exclusively for schizophrenia, the network provides support and resources for people who experience auditory hallucinations, which are common in schizophrenia
Summary
Schizophrenia is a challenging mental health disorder that requires a multidimensional approach for effective management. Early diagnosis, appropriate treatment, and ongoing support can significantly improve the quality of life for individuals living with schizophrenia. By raising awareness, reducing stigma, and providing comprehensive care, we can promote understanding, compassion, and better outcomes for individuals and their families affected by schizophrenia.
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.