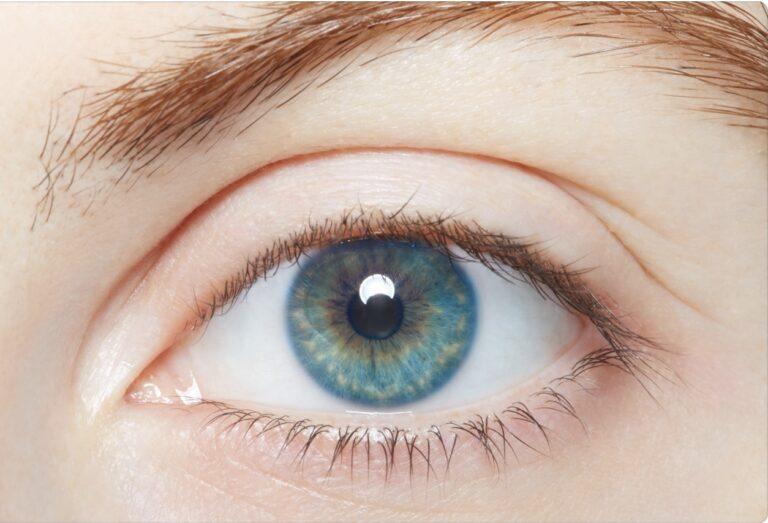
Glaucoma
Get valuable insights into Glaucoma, including its causes, symptoms, prevention strategies, and treatment options, while also learning about how you can lower the cost of the medications used to treat Glaucoma.
MEDICAL INFORMATION
Glaucoma Key Facts
Related Medications
Glaucoma is a complex eye disease that affects the optic nerve and can lead to vision loss if left untreated. This comprehensive article aims to provide an overview of glaucoma, including its causes, types, symptoms, risk factors, diagnostic methods, and available treatment options.
What is glaucoma?
Glaucoma refers to a group of eye conditions characterized by damage to the optic nerve, which is responsible for transmitting visual information from the eye to the brain. The most common type of glaucoma is primary open-angle glaucoma, but other types include angle-closure glaucoma and normal-tension glaucoma.
What are the causes and risk factors of glaucoma?
The exact cause of glaucoma is not fully understood, but there are several known risk factors that contribute to its development. It is important to note that having one or more risk factors does not necessarily mean that an individual will develop glaucoma, but they increase the likelihood. The causes and risk factors of glaucoma include:
- Elevated Intraocular Pressure (IOP): Elevated intraocular pressure (eye pressure) is the most significant risk factor for glaucoma. It is usually caused by a build up of fluid in the front part of the eye. The pressure inside the eye (intraocular pressure) is normally regulated to maintain a balance. When the pressure exceeds normal eye pressure, it can damage the optic nerve and lead to glaucoma
- Family History: Having a family history of glaucoma increases the risk of developing the condition. There is a genetic component to glaucoma, and certain gene variations have been associated with an increased susceptibility to the disease
- Age: The risk of glaucoma increases with age. While glaucoma can affect individuals of all age groups, the incidence rises significantly after the age of 40, and the risk continues to increase with advancing age
- Ethnicity: Certain ethnic groups, such as African-Americans, Hispanics, and Asians, have a higher risk of developing certain types of glaucoma, such as primary open-angle glaucoma (POAG) and angle-closure glaucoma
- Structural Abnormalities of the Eye: Structural abnormalities in the eye can increase the risk of glaucoma. For example, individuals with thinner corneas or an unusually shaped or narrow drainage angle in the eye are more prone to developing certain types of glaucoma, such as angle-closure glaucoma
- Medical Conditions: Certain medical conditions, such as diabetes, hypertension (high blood pressure), and hypothyroidism, have been associated with an increased risk of glaucoma. Additionally, conditions that cause poor blood flow to the optic nerve, such as migraines, may also contribute to the development of glaucoma
- Prolonged Use of Steroid Medications: Long-term use of corticosteroid medications, whether in the form of eye drops, inhalers, or oral medications, can increase the risk of glaucoma. This is more likely to occur with higher doses and longer durations of use
- Eye Injuries or Surgery: Previous eye injuries, trauma, or certain types of eye surgery may increase the risk of glaucoma. Inflammation or changes in the eye’s anatomy caused by these factors can disrupt the normal flow of fluid in the eye and lead to increased intraocular pressure
- Other Factors: Other factors that may increase the risk of glaucoma include a history of severe nearsightedness (myopia), prolonged use of certain medications (such as antihistamines and decongestants), and a history of previous retinal detachment or other eye conditions
It is important to note that while these risk factors are associated with an increased likelihood of developing glaucoma, the condition can still occur in individuals without any known risk factors. Regular eye examinations and screenings are essential for early detection and appropriate management of glaucoma, especially for individuals with one or more risk factors.
What are the symptoms of glaucoma?
Glaucoma, a leading cause of blindness, is often referred to as the “silent thief of sight” because it typically does not cause noticeable symptoms in its early stages. The vision loss associated with glaucoma is gradual and usually starts with the peripheral (side) vision. As the disease progresses, it can lead to more significant vision impairment and, if left untreated, eventual blindness. However, certain types of glaucoma can have symptoms that indicate the presence of the condition. The symptoms of glaucoma include:
Open-angle glaucoma (the most common form of glaucoma)
- No early symptoms: In the early stages, open-angle glaucoma usually does not cause noticeable symptoms. Vision remains relatively unaffected, making it challenging to detect the disease without regular eye examinations
- Gradual loss of peripheral vision: As open-angle glaucoma progresses, it gradually affects the peripheral vision (side vision). This can result in a condition called “tunnel vision” where the person’s field of view narrows
- Impaired night vision: Some individuals with open-angle glaucoma may experience difficulty seeing in low-light conditions or at night
- blind spots
Acute angle-closure glaucoma (less common but more symptomatic)
- Severe eye pain: Acute angle-closure glaucoma, also called closed-angle glaucoma or narrow-angle glaucoma, often presents with sudden and severe eye pain, which can be accompanied by a headache. The pain may be described as a sharp, intense, or deep ache
- Blurred or hazy vision: The affected eye may experience blurred vision or a loss of clarity. This symptom may be intermittent, occurring during episodes of increased intraocular pressure
- Halos around lights: Individuals with acute angle-closure glaucoma may notice the presence of halos or rainbow-colored rings around lights, especially in dimly lit environments
- Redness and swelling of the eye: The eye may appear red, swollen, and may feel tender to touch
- Nausea and vomiting: In some cases, acute angle-closure glaucoma can cause accompanying symptoms such as nausea and vomiting
Congenital glaucoma (less common but more symptomatic)
- This condition, also referred to as newborn glaucoma, is characterized by the child being born with an enlargement of the eyes or the enlargement being observed within the first month of life. It’s thought that the increase in intraocular pressure (IOP) actually begins while the child is still in the womb
How is glaucoma diagnosed?
The diagnosis of glaucoma involves a comprehensive evaluation of the eye, including a thorough medical history, visual acuity testing, and several specialized tests. The goal of the eye exam is to assess the health of the optic nerve, measure intraocular pressure (IOP), evaluate visual field function, and examine the structures of the eye. The process of diagnosing glaucoma typically involves the following steps:
Medical history
- The healthcare professional, or eye doctor, will begin by taking a detailed medical history, including information about symptoms, family history of glaucoma, previous eye conditions or surgeries, and any medications being taken
Eye examination
- A comprehensive eye examination will be performed, which includes measuring visual acuity to assess overall vision
- Glaucoma can be detected in its early stages through a dilated eye exam. During this exam, drops are placed in the eyes to dilate, or widen, the pupils. The healthcare professional will then examine the structures of the eye and assess the health of the cornea, lens, retina and optic nerve for signs of damage and other possible problems
Measurement of intraocular pressure (IOP)
- The intraocular pressure is measured using a tonometer. There are various types of tonometers available, including non-contact tonometry and applanation tonometry
- Non-contact tonometry uses a puff of air to measure the IOP, while applanation tonometry involves applying gentle pressure to the cornea using a calibrated instrument
Assessment of optic nerve
- The healthcare professional will evaluate the appearance of the optic nerve using a specialized instrument called an ophthalmoscope or a slit lamp with a special lens. This examination helps identify any signs of optic nerve damage, such as cupping or thinning of the optic nerve fibers
Visual field testing
- Visual field testing assesses peripheral vision and helps detect any areas of vision loss
- Perimetry is the most commonly used test for visual field assessment. It involves staring at a central point while responding to visual stimuli presented at different locations in the visual field
Imaging tests
- Imaging tests, such as optical coherence tomography (OCT) or scanning laser polarimetry, may be performed to obtain detailed images of the optic nerve and measure the thickness of the nerve fibers
- These tests provide quantitative data and help monitor changes in the optic nerve over time
Gonioscopy
- Gonioscopy is a procedure that examines the drainage angle of the eye. It involves placing a special lens on the cornea to visualize the angle structures
- This test is particularly useful for diagnosing angle-closure glaucoma and determining the type of glaucoma present
Based on the findings from these examinations and tests, the healthcare professional can make a diagnosis of glaucoma. It is important to note that glaucoma is a progressive disease, and a single examination may not always be sufficient to confirm the presence of the condition. Regular follow-up visits and repeat testing may be necessary to monitor the optic nerve health, IOP, and visual field function over time.
Early detection and diagnosis are crucial for the effective management of glaucoma. Regular eye examinations, especially for individuals with risk factors or a family history of glaucoma, are essential to detect the condition in its early stages when treatment can be most effective in preserving vision. If allowed to progress, glaucoma can advance from affecting peripheral or side vision to causing central vision loss.
What are glaucoma treatment options?
The goal of treatment options for glaucoma is to lower intraocular pressure (IOP), preserve vision, and prevent further damage to the optic nerve. The choice of treatment depends on the type and severity of glaucoma, as well as the individual’s overall health. The main treatment options for glaucoma include:
Eye drops
- Medications in the form of eye drops are commonly prescribed as the first-line treatment for glaucoma. These eye drops work by either reducing the production of aqueous humor (the fluid inside the eye) or improving its drainage
- Common types of eye drops for glaucoma include prostaglandin analogs, beta-blockers, alpha-adrenergic agonists, and carbonic anhydrase inhibitors
- It is crucial to follow the prescribed regimen and properly administer the eye drops as directed by the healthcare professional
Oral medications
- In some cases, oral medications may be prescribed to treat glaucoma alongside or as an alternative to eye drops to reduce high eye pressure. These medications work by reducing the production of aqueous humor or improving its outflow
- Oral carbonic anhydrase inhibitors are an example of such medications
Laser therapy
- Laser trabeculoplasty: This procedure uses a laser to enhance the drainage of fluid from the eye. It is typically performed in open-angle glaucoma. The laser is focused on the drainage angle, stimulating the trabecular meshwork to improve fluid flow
- Laser peripheral iridotomy: This procedure is performed in angle-closure glaucoma. A small hole is created in the iris using a laser, allowing fluid to bypass the blocked drainage angle and reducing the risk of an acute attack
Microsurgery
- Trabeculectomy: This surgical procedure creates a new drainage channel for the aqueous humor by removing a small piece of the eye’s drainage system (trabecular meshwork). It is typically used in open-angle glaucoma when medications and laser therapy are not effective
- Glaucoma drainage devices: In some cases, a small tube or shunt is implanted in the eye to improve the drainage of fluid and lower IOP. This option is often considered for more complex or advanced cases of glaucoma
- Minimally invasive glaucoma surgery (MIGS): These procedures involve implanting small devices or making tiny incisions to enhance the outflow of fluid and lower IOP. MIGS procedures are typically less invasive than traditional surgery and may be suitable for certain types of glaucoma
Combination therapy
- Depending on the severity and progression of glaucoma, a combination of different treatment modalities may be used to effectively manage the condition. This can include a combination of eye drops, laser therapy, and surgical procedures
- The choice of treatment for glaucoma is highly individualized, and it is important to work closely with a healthcare professional to determine the most appropriate treatment plan based on the specific characteristics of the glaucoma and the individual’s overall health. Early detection, regular eye examinations, and adherence to prescribed treatment regimens are key to preserving vision and managing glaucoma effectively
What medications are used in glaucoma?
Prostaglandin Analogs
- Latanoprost
- Travoprost
- Bimatoprost
- Tafluprost
- Unoprostone
Beta-Blockers
- Timolol
- Betaxolol
- Levobunolol
- Carteolol
Carbonic Anhydrase Inhibitors (CAIs)
- Dorzolamide
- Brinzolamide
- Acetazolamide (also available in oral form for certain cases)
Alpha-Agonists
- Brimonidine
- Apraclonidine
Rho Kinase Inhibitor
- Netarsudil
Miotic Agents
- Pilocarpine
- Carbachol
Lifestyle and self-care
Certain lifestyle modifications can help manage glaucoma, such as:
- Regular eye examinations and follow-ups
- Compliance with prescribed medications and treatments
- Protecting the eyes from injury or trauma
- Maintaining a healthy lifestyle, including exercise and a balanced diet
- Managing other medical conditions, such as diabetes and hypertensionSummary
Glaucoma is a progressive eye disease that requires early detection and ongoing management to preserve vision. Regular eye exams, understanding the risk factors, and prompt treatment are vital. If you experience any symptoms or are at risk for glaucoma, consult an eye care professional for a comprehensive evaluation and appropriate management strategies. With timely diagnosis and appropriate treatment, the progression of glaucoma can be slowed or halted, helping to maintain good visual health and quality of life.
What glaucoma support organizations are there available to support me in the UK?
- International Glaucoma Association (IGA): The International Glaucoma Association is a leading charity organization in the UK that supports individuals with glaucoma. They provide information resources, a helpline, online support forums, educational materials, and awareness campaigns
- Glaucoma UK: Glaucoma UK is a charity organization dedicated to providing support and raising awareness about glaucoma. They offer information resources, support groups, online forums, educational events, and fundraising initiatives
- Royal National Institute of Blind People (RNIB): The RNIB is a UK-based charity organization that supports individuals with visual impairments, including those with glaucoma. They provide information resources, helplines, local support services, and advocacy initiatives
- Fight for Sight: Fight for Sight is a charity organization that funds research into various eye conditions, including glaucoma. They provide information resources, research updates, and support initiatives aimed at preventing sight loss
- Macular Society: Although primarily focused on macular conditions, the Macular Society offers support and resources for individuals with various eye conditions, including glaucoma. They provide information materials, helplines, support groups, and fundraising events
What glaucoma support organizations are there available to support me in the US?
- Glaucoma Research Foundation (GRF): The Glaucoma Research Foundation is a national non-profit organization that focuses on funding research and providing education about glaucoma. They offer information resources, educational materials, support networks, and research updates
- American Glaucoma Society (AGS): The American Glaucoma Society is a professional organization comprised of ophthalmologists specializing in glaucoma. Their website provides information on glaucoma, patient education resources, and a directory to help individuals find glaucoma specialists
- National Eye Institute (NEI): The National Eye Institute is a division of the U.S. National Institutes of Health (NIH) that supports research and provides information on various eye conditions, including glaucoma. Their website offers resources, research updates, clinical trial information, and educational materials
- Prevent Blindness: Prevent Blindness is a national non-profit organization that focuses on preventing vision loss and promoting eye health. They offer resources, educational materials, advocacy initiatives, and support networks for individuals with various eye conditions, including glaucoma
- Glaucoma Foundation: The Glaucoma Foundation is a non-profit organization that supports research, education, and patient care for glaucoma. They provide information resources, research updates, and educational programs
Summary
Glaucoma is a progressive eye disease that requires early detection and ongoing management to preserve vision. Regular eye examinations, understanding the risk factors, and prompt treatment are vital. If you experience any symptoms or are at risk for glaucoma, consult an eye care professional for a comprehensive evaluation and appropriate management strategies. With timely diagnosis and appropriate treatment, the progression of glaucoma can be slowed or halted, helping to maintain good visual health and quality of life.
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.