Glaucoma is a condition that affects the eyes and can lead to loss of vision if not treated. It is caused by an increase in pressure inside the eye and can lead to vision loss if left untreated. While there is no cure for glaucoma, it can be managed with medication and glaucoma surgery. In this post, we will explore the causes and symptoms of glaucoma. We hope this information will help our readers better understand this condition and seek treatment if they feel they may be affected.
What is glaucoma?
Glaucoma is an eye condition that affects eye health and decreases the ability to see things effectively. It is one of the leading causes of blindness. It usually occurs when fluid in your eye does not drain properly, causing pressure to build up and damage the optic nerve. This high eye pressure (intraocular pressure) is often caused by an imbalance between the production of aqueous humor, which is a clear liquid that provides nourishment to the eyeball and the drainage of this fluid from your eye. A decrease in blood flow can also lead to the development of glaucoma, as it reduces the body’s ability to take away waste products. Treating glaucoma involves managing these levels of fluid, drainage and circulation in order to protect your eyesight and vision health.
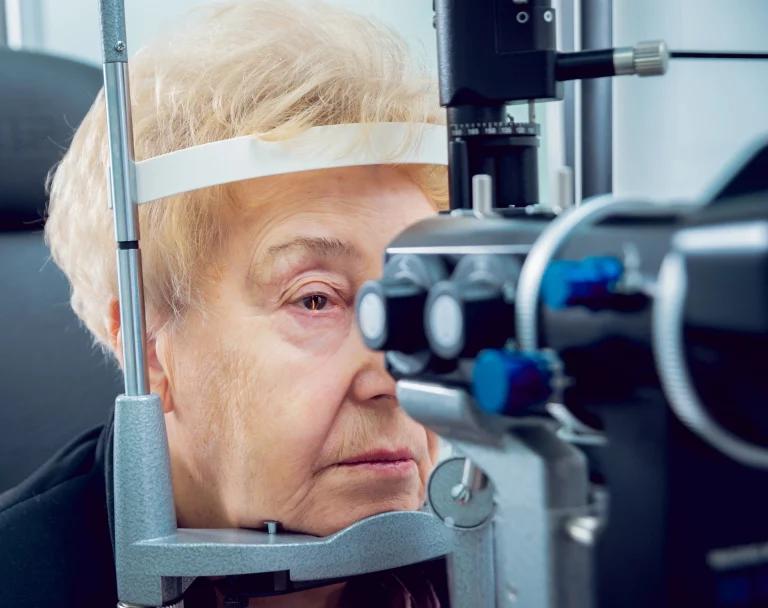
As with all eye diseases, seeking prompt medical attention can help manage symptoms in the early stages. Early detection through regular eye examinations is essential for controlling glaucoma and preventing further eye damage or vision loss. Taking care of your eye health is key to maintaining good sight, so make sure you get regular check-ups with your eye doctor.
There are two different types of glaucoma: open-angle glaucoma and angle-closure glaucoma. Open-angle glaucoma is the most common type of glaucoma, it develops slowly over time without causing any pain. Angle-closure glaucoma happens when the angle between your iris and cornea becomes narrow, causing a sudden increase in pressure inside your eye. Angle-closure glaucoma can be a medical emergency because it can lead to permanent vision loss in a short period of time.
Symptoms of Glaucoma
Primary open-angle glaucoma
Open-angle glaucoma is the most common form of glaucoma affecting millions of Americans. The cause of open-angle glaucoma is unknown, but it is associated with a buildup of pressure in the eye. This pressure can damage the optic nerve, which transmits signals from the eye to the brain. Over time, open-angle glaucoma can lead to blindness. Early diagnosis and treatment are essential to prevent vision loss.
There are no early symptoms of open-angle glaucoma, which is why regular eye exams are so important. However, as the disease progresses, symptoms may include:
- Loss of peripheral vision and blind spots
- Difficulty adjusting to changes in light
- Difficulty seeing at night
- Halos around lights
- Pain or red eyes
Acute angle-closure glaucoma (also called “closed-angle glaucoma” or “narrow-angle glaucoma”)
Angle-closure glaucoma is a type of glaucoma that occurs when the angle between the iris and the cornea becomes narrower, blocking the normal flow of fluid out of the eye. This can cause an increase in pressure inside the eye, which can damage the optic nerve. Angle-closure glaucoma is a medical emergency and needs to be treated immediately.
The most common symptom of angle-closure glaucoma is a sudden onset of severe eye pain. Other symptoms may include nausea and vomiting, headache, blurred vision and rainbow-coloured halos around lights.
If you experience any of these symptoms, you should see an ophthalmologist or seek emergency help. Early diagnosis and treatment are essential to prevent vision loss from angle-closure glaucoma.
If you experience any of these symptoms, it is important to see an eye doctor immediately.
Less common types of glaucoma
Congenital glaucoma occurs when the pupil does not form properly or does not drain correctly during infancy, leading to a buildup of pressure in the eye.
Secondary glaucoma is caused by already existing conditions such as diabetes, cataracts or trauma to the eye causing added pressure to the eye.
Normal-tension glaucoma occurs even when there is normal eye pressure. It usually develops slowly, making it difficult to diagnose early on.
Pigmentary glaucoma is caused by tiny flecks of pigment from the iris clogging the drainage angles in the eye and preventing fluid from leaving.
Exfoliative glaucoma occurs when proteins build up in the eye leading to high pressure in the intraocular area.
What causes glaucoma?
Glaucoma is caused by increased pressure within the eye. It can cause optic nerve damage, leading to vision problems like tunnel vision or blindness. There are two primary causes of glaucoma: elevated fluid pressure inside the eye and damage to the optic nerve from other diseases, such as diabetes or high blood pressure. In some cases, glaucoma is caused by a combination of these factors.
There are other factors associated with glaucoma which can also contribute to the mechanics of this condition. Risk factors for glaucoma can include:
- Family history: People with a family history of glaucoma have a greater chance of developing the condition
- Age: Glaucoma is most common in adults over the age of 60
- Race: African Americans have a higher risk of developing glaucoma than any other racial group
- Medical conditions: Diabetes and high blood pressure (hypertension) are two medical conditions that increase your risk of glaucoma
- Eye injuries: Traumatic injuries to the eye can increase your risk of developing glaucoma later in life
- Medications: Some medications can increase the pressure in your eyes and lead to glaucoma. These include corticosteroids, beta-blockers and anticholinergics
- Previous eye surgery: Certain types of eye surgery can increase your risk of developing glaucoma later on
How is glaucoma diagnosed?
Visual Field Test
There are several tests that can be used for glaucoma diagnosis. The most common is a visual field test. When it comes to glaucoma diagnosis, a visual field test is used to assess the extent of your peripheral vision. During the test, you will be seated in front of a bowl-shaped device and asked to look straight ahead. As different shapes and patterns are flashed in various locations across your field of vision, you’ll need to press a button whenever something appears. This helps the doctor determine if you have any blind spots within your peripheral vision due to nerve damage – a potential sign of glaucoma. This quick and easy test can help detect and prevent further damage from occurring in order to protect your eyesight. Although some patients may find it uncomfortable when bright lights are exposed directly to their eyes, it usually only takes several minutes to complete and no preparation is required beforehand.
Tonometry test
The tonometry test, also known as an eye pressure test, is one of the most important diagnostic tests for glaucoma. It helps us to measure the amount of pressure that is building up inside our eyes. During the procedure, a small device applies a light touch to your eye which helps to measure the internal pressure. Additionally, it may be done in combination with other tests such as an eye examination, imaging studies and visual field tests to diagnose glaucoma. This test is quick and painless and is important for protecting your eyesight now and in the future.
Glaucoma treatment
There are different glaucoma treatment options available. Initially, an optometrist or ophthalmologist may recommend changes to lifestyle such as avoiding certain medications or using protective sunglasses outdoors. Depending on how advanced your glaucoma is and the cause of the build-up in pressure, treatment may range from medication to laser surgery.
Medication
Medications are the most common type of treatment for glaucoma and may include eye drops that help reduce pressure within the eye or prescription pills to improve drainage of fluid from inside the eye. Eye drops often need to be used several times a day, whereas medications taken orally only require one dose per day. Speak with your healthcare provider to determine if either of these types of medications is right for you. Taking your medications correctly is crucial in keeping your eyes healthy and protected.
Surgery
Laser surgery can offer a way to help manage glaucoma. Amongst the surgical options available are two main types of laser treatment: Iridotomy and Trabeculoplasty. Both have been developed to reduce pressure inside the eye.
Iridotomy is a type of laser surgery that widens drainage pathways near the iris (coloured part of the eye) so that fluid can pass through more easily. Trabeculoplasty, on the other hand, uses laser energy to create tiny burns in specific areas around an eye’s trabecular meshwork – an area where fluid passes out of the eye.
Trabeculectomy is a common surgical procedure also used to treat glaucoma. It involves creating a tiny hole in the eye, which helps allow fluid to flow and relieve pressure inside the eye that could potentially damage the optic nerve if not treated. This outpatient procedure can lower levels of intraocular (eye) pressure, providing much-needed relief from pain and other symptoms associated with glaucoma.
Your eye doctor will explain the risks and benefits of having surgery versus using medications to control your glaucoma, so you can make an informed decision about which treatment path is best for you, based on your individual needs.
What are some preventative measures to take to avoid developing glaucoma?
First and foremost, visiting an eye care professional on a regular basis is a great preventative measure. During these visits, they will be able to look for signs of glaucoma in the back of your eyes and give additional advice based on whatever other risk factors you might possess, such as family history or if you have a pre-existing condition like diabetes or high blood pressure.
Eating a healthy diet that includes plenty of fruits and vegetables can also help reduce the risk since many studies have shown that those with inadequate nutrition are more likely to develop glaucoma. Other changes in lifestyle such as avoiding prolonged exposure to extremely bright light and reducing overall screen time are useful too.
Furthermore, it’s important to get plenty of rest. Good sleep hygiene is key to so many aspects of healthful living. Finally, it’s important not to smoke, as it can raise your intraocular pressure (IOP), which may increase your risk of developing glaucoma. Taking these preventative measures before symptoms occur could make all the difference in sustaining excellent vision now and into the future!
If you have any of the symptoms or risk factors of glaucoma, it is important to speak to a healthcare professional right away so that you can be diagnosed and treated for glaucoma. With early diagnosis and treatment, you can slow or stop the progression of glaucoma and preserve your vision.
Sources
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.