Bacterial Infections
Get valuable insights into Bacterial Infections, including its causes, symptoms, prevention strategies, and treatment options, while also learning about how you can lower the cost of the medications used to treat Bacterial Infections.

MEDICAL INFORMATION
Bacterial Infections Key Facts
Related Medications
Bacterial infections are common ailments caused by the invasion of harmful bacteria into the body. These infections can affect various parts of the body, ranging from the skin to the respiratory system, urinary tract, and beyond. Understanding the causes, types, symptoms, and treatment options for bacterial infections is essential for proper diagnosis, effective management, and prevention of complications.
What is the definition of a bacterial infection?
Bacteria are single-celled microorganisms that can cause a wide range of infections, affecting different parts of the body such as the skin, respiratory system, urinary tract, gastrointestinal tract, and more. Infections can occur when bacteria enter the body through various routes, including direct contact with infected individuals, exposure to contaminated objects, or ingestion of contaminated food or water.
What are the different types of infectious diseases?
Bacterial infections can affect various parts of the body, leading to different types of infections. Here are some common types of bacterial infections:
Skin Infections
- Cellulitis: A bacterial infection affecting the deeper layers of the skin, often causing redness, swelling, warmth, and pain
- Impetigo: A highly contagious infection that commonly affects children, causing red sores or blisters that ooze and form yellowish crusts
- Boils: Painful, pus-filled bumps that develop in hair follicles or oil glands
Respiratory Infections
- Pneumonia: Infection of the lungs, leading to symptoms such as cough, fever, chest pain, and difficulty breathing
- Sinusitis: Inflammation and infection of the sinus cavities, causing nasal congestion, facial pain, and sinus pressure
- Bronchitis: Infection of the bronchial tubes, resulting in cough, mucus production, and chest discomfort
Urinary Tract Infections (UTIs)
- Bladder Infection (Cystitis): Infection of the bladder, leading to frequent urination, pain or burning during urination, and cloudy urine
- Kidney Infection (Pyelonephritis): Infection of the kidneys, causing back or side pain, fever, chills, and urinary symptoms
Gastrointestinal Infections
- Food Poisoning: Bacterial contamination of food, leading to symptoms like nausea, vomiting, abdominal pain, and diarrhea
- Gastroenteritis: Inflammation and infection of the gastrointestinal tract, causing diarrhea, abdominal cramps, and sometimes vomiting
Sexually Transmitted Infections (STIs)
- Chlamydia: A common bacterial STI that can cause genital infections and may lead to complications if left untreated
- Gonorrhoea: Another bacterial STI that primarily affects the genital tract but can also cause infections in other parts of the body
- Syphilis: A systemic bacterial infection that can progress through different stages and affect various organs if untreated
Bloodstream Infections
Sepsis: A severe infection that spreads through the bloodstream, potentially leading to organ dysfunction and life-threatening complications
Wound Infections
Infections that develop in wounds, surgical sites, or cuts, which can vary in severity depending on the bacteria involved
It’s important to note that this list represents only a selection of common bacterial infections, and there are many other types and subtypes of bacterial infections that can occur. Proper diagnosis and treatment by healthcare professionals are crucial to effectively manage bacterial infections and prevent complications.
What are the causes of bacterial infections?
Bacterial infections are caused by the presence and growth of harmful bacteria in or on the body. There are millions of different types of bacteria, most of which are harmless to humans. Some even help with bodily functions such as digestion. However, certain types of bacteria can cause diseases when they invade the human body. Here are some common ways these harmful bacteria can cause infections:
Direct contact examples
Bacterial infections can spread through direct contact, either person-to-person (such as through touching, kissing, or sexual intercourse) or by contact with surfaces contaminated with bacteria. Examples include skin infections (like impetigo) or sexually transmitted diseases (like gonorrhea)
Indirect contact
This typically happens when an individual comes into contact with a contaminated surface and then touches their face, mouth, or eyes
Inhalation
Respiratory infections can occur when a person inhales bacteria present in airborne droplets from a cough or sneeze. Examples include tuberculosis and pneumonia
Ingestion
Consuming contaminated food or water can lead to bacterial infections in the digestive system. Examples include salmonella or E. coli infections
Bites and wounds
An open wound can provide a pathway for bacteria to enter the body. Animal or insect bites can also transmit bacteria. Examples include tetanus or Lyme disease
Medical procedures
Sometimes, bacteria can enter the body during surgical or medical procedures, leading to infections like urinary tract infections from catheters, or surgical site infections
It’s important to note that susceptibility to bacterial infections can depend on various factors including the strength of a person’s immune system, their age, and the presence of other medical conditions. The body has numerous defense mechanisms to prevent and combat bacterial infections, but when these defenses are compromised or overwhelmed, a bacterial infection can occur.
What are the signs and symptoms of bacterial infections?
The symptoms of a bacterial infection can vary depending on the type of infection and the specific area of the body affected. However, there are some common symptoms that may indicate a bacterial infection.
Fever
A bacterial infection can often cause an elevated body temperature, resulting in fever. This is the body’s natural response to fighting off the infection
Pain and Inflammation
Bacterial infections can lead to localized pain, redness, and swelling in the affected area. This can occur in various parts of the body, such as the skin, throat, sinuses, urinary tract, or joints
Fatigue and Malaise
Feeling tired, weak, or generally unwell is a common symptom of many bacterial infections. The body’s immune response to the infection can drain energy levels and cause overall discomfort
Respiratory Symptoms
Bacterial respiratory infections, such as pneumonia or bronchitis, may cause symptoms like coughing, chest pain, shortness of breath, or difficulty breathing
Gastrointestinal Symptoms
Bacterial infections in the gastrointestinal tract can result in symptoms such as nausea, vomiting, abdominal pain, cramping, diarrhea, or changes in bowel movements
Urinary Symptoms
Bacterial urinary tract infections (UTIs) can cause frequent urination, pain or a burning sensation during urination, cloudy or bloody urine, and an urgent need to urinate
Skin Symptoms
Skin infections caused by bacteria may present with symptoms like redness, warmth, tenderness, swelling, or the presence of pus-filled lesions, such as boils or abscesses
It is important to note that these symptoms are general and can overlap with those of other conditions. Proper diagnosis by a healthcare professional, through physical examination, medical history assessment, and sometimes laboratory tests, is necessary to determine the specific cause and type of bacterial infection. Early detection and appropriate treatment can help manage bacterial infections effectively and prevent complications.
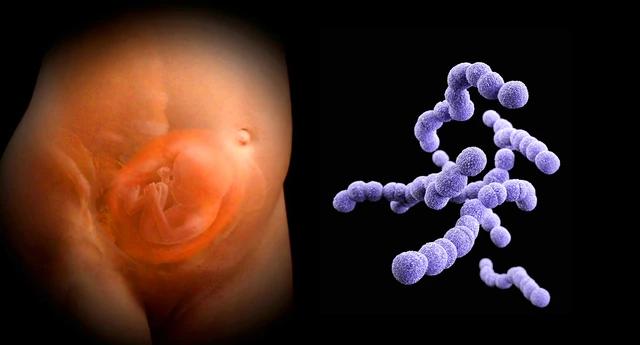
What is the most common bacteria that causes Bacterial Infections?
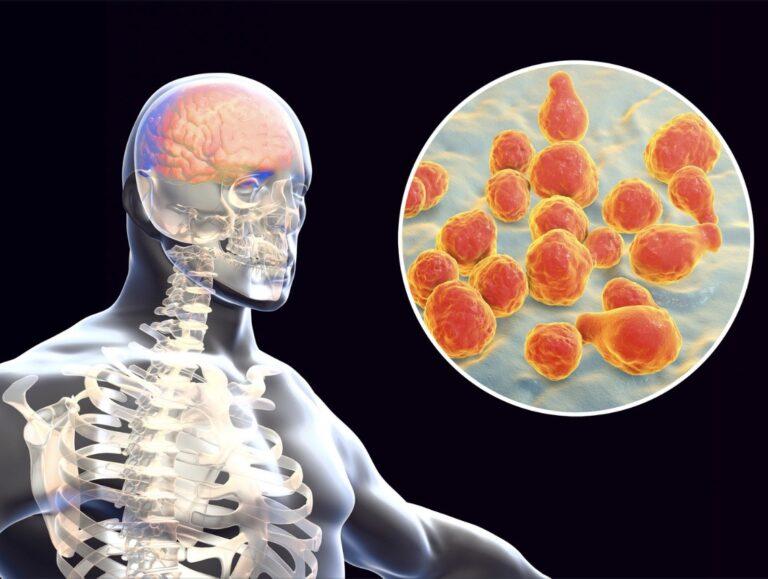
Streptococcus is a genus of gram-positive bacteria that can cause a wide range of infections in humans. Here’s how it can cause infections:
Respiratory transmission
Streptococcus pneumoniae, one of the most common species, is a leading cause of pneumonia. It spreads through respiratory droplets when an infected person coughs or sneezes. In addition to pneumonia, it can also cause ear and sinus infections, as well as meningitis
Direct contact
Streptococcus pyogenes, also known as Group A Streptococcus (GAS), can cause infections like strep throat and skin infections (impetigo). It spreads through direct contact with mucus from the nose or throat of infected persons or through contact with infected wounds or sores on the skin
Foodborne transmission
Group B Streptococcus (GBS or Streptococcus agalactiae) can sometimes cause foodborne illness, although it’s more commonly known for causing infections in newborns and in adults with compromised immune systems
Mother to child transmission
GBS can also be passed from a mother to her baby during childbirth, potentially causing serious infections in the newborn such as sepsis, pneumonia, and meningitis
Other common bacteria include staphylococcus aureus and E.Coli
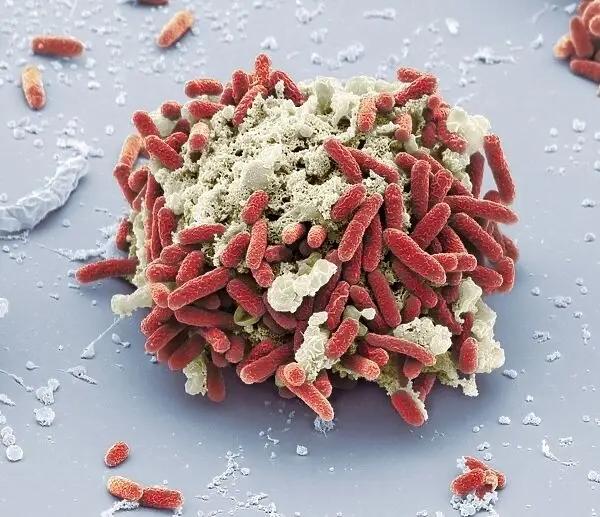
What is MRSA?
MRSA, or Methicillin-Resistant Staphylococcus Aureus, is a type of bacterium that’s resistant to several widely used antibiotics, including methicillin, making infections with MRSA harder to treat.
Staphylococcus aureus (S. aureus) is a common bacterium that’s often carried on the skin or in the nose and throat, and it’s generally harmless. However, if it enters the body through a cut or wound, it can cause a range of infections, which can be mild or potentially life-threatening.
Methicillin was once used to treat S. aureus infections, but the bacterium has since developed resistance to methicillin and other similar antibiotics, including oxacillin, penicillin, and amoxicillin.
There are two main types of MRSA infection
- Hospital-acquired MRSA (HA-MRSA): This occurs in healthcare settings, such as hospitals or nursing homes. It can cause severe and potentially life-threatening infections, such as bloodstream infections, pneumonia, or surgical site infections
- Community-acquired MRSA (CA-MRSA): This occurs in the wider community — among healthy people — and is often spread through skin-to-skin contact. It typically causes skin infections, such as boils or abscesses
Preventive measures include good hygiene practices, like regular hand washing, keeping wounds clean and covered, and not sharing personal items such as towels or razors. It’s also important to use antibiotics only as directed by healthcare professionals to help prevent antibiotic resistance.
What are the treatment options for bacterial infections?
The treatment options for bacterial infections primarily involve the use of antibiotics, which are medications specifically designed to target and kill bacteria. The choice of antibiotics depends on the type of bacterial infection, the severity of symptoms, the location of the infection, and the individual’s overall health.
Antibiotics
- Broad-Spectrum Antibiotics: These antibiotics are effective against a wide range of bacteria and are commonly prescribed when the specific bacteria causing the infection is unknown or when the infection is severe
- Narrow-Spectrum Antibiotics: These antibiotics target specific types of bacteria and are prescribed when the causative bacteria are identified through laboratory tests or when the infection is localized to a specific area
Duration of Treatment
The duration of antibiotic treatment can vary depending on the type and severity of the infection. It is important to complete the full course of antibiotics as prescribed by the healthcare professional, even if symptoms improve before the treatment period ends. This helps ensure the complete eradication of bacteria and prevents the development of antibiotic resistance
Supportive Care
In addition to antibiotics, supportive care measures may be recommended to help manage symptoms and promote recovery. These may include rest, adequate hydration, over-the-counter pain relievers, warm compresses, or topical ointments for localized infections
Prevention and Hygiene
Preventive measures are crucial to reduce the risk of bacterial infections. These may include practicing good hygiene, such as frequent hand-washing, covering the mouth and nose when coughing or sneezing, and properly handling and storing food. Vaccinations are also available for certain bacterial infections, such as tetanus or pneumonia
It is important to note that not all bacterial infections require antibiotic treatment. Some mild infections may resolve on their own, while others, such as viral infections, do not respond to antibiotics. Healthcare professionals can provide accurate diagnosis and determine the appropriate treatment based on the specific circumstances.
It is essential to follow the advice of healthcare professionals, complete the prescribed treatment, and attend follow-up appointments to ensure effective management of bacterial infections and prevent complications.
What are the complications of bacterial infections?
Bacterial infections, if left untreated or not properly managed, can lead to various complications. The severity and nature of these complications depend on factors such as the type of infection, location, the overall health of the individual, and the timely administration of appropriate treatment. Here are some potential complications that can arise from bacterial infections
Spread of Infection
Bacterial infections can spread to nearby tissues, organs, or the bloodstream, leading to a condition known as sepsis. Sepsis is a life-threatening systemic response to infection that can cause organ dysfunction, septic shock, and even death
Abscess Formation
Untreated bacterial infections, particularly skin infections or deep tissue infections, can result in the formation of abscesses. Abscesses are localized collections of pus that may require drainage or surgical intervention
Chronic or Recurrent Infections
In some cases, bacterial infections can become chronic or recurrent, persisting or recurring despite treatment. This can occur due to antibiotic resistance or the presence of certain bacterial strains that are difficult to eradicate
Damage to Organs or Tissues
Bacterial infections affecting specific organs or tissues, such as the lungs, kidneys, heart valves, or joints, can result in damage or dysfunction if not promptly treated. For example, untreated pneumonia can lead to lung complications, while untreated urinary tract infections can potentially cause kidney damage
Secondary Infections
Bacterial infections can weaken the immune system, making individuals more susceptible to secondary infections. These secondary infections can be caused by different bacteria or even fungi, further complicating the treatment and recovery process
Post-Infectious Complications
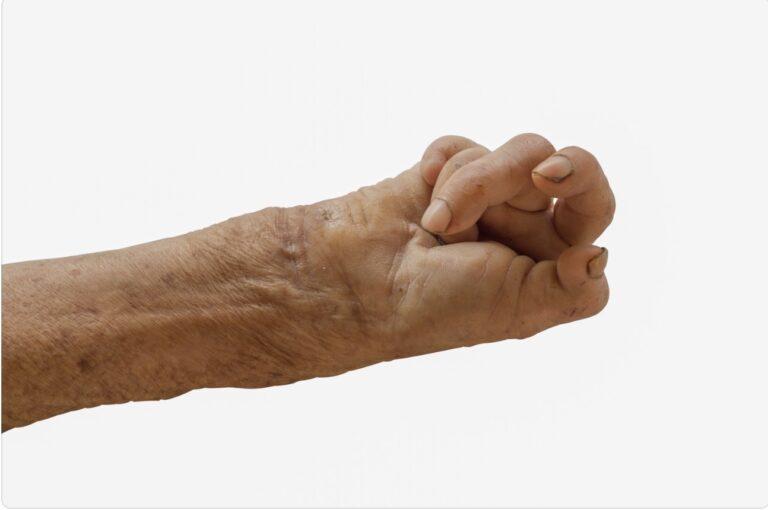
Some bacterial infections can trigger post-infectious complications, which are immune-mediated or inflammatory responses that occur after the initial infection has resolved. Examples include rheumatic fever following streptococcal infection or reactive arthritis following certain gastrointestinal or genitourinary infections
Long-Term Health Effects
In certain cases, bacterial infections can have long-term effects on overall health. For example, untreated or recurrent streptococcal infections can lead to complications such as rheumatic heart disease or kidney damage
Prompt diagnosis, appropriate treatment, and adherence to prescribed medications are crucial for preventing or minimizing the risk of complications associated with bacterial infections. It is important to seek medical attention if symptoms worsen, persist, or if there are signs of severe infection, such as high fever, rapid breathing, confusion, or severe pain
What medications are used to treat bacterial infections?
Bacterial infections are typically treated with antibiotics, which are medications specifically designed to target and kill bacteria. The choice of antibiotic depends on several factors, including the type of bacterial infection, the specific bacteria causing the infection, the severity of symptoms, and any known antibiotic resistance patterns. Here are some commonly used antibiotics for the treatment of bacterial infections:
Penicillins
- Penicillin: Effective against a wide range of bacteria, it is commonly used for respiratory tract infections, skin infections, and certain sexually transmitted infections
- Amoxicillin: A broad-spectrum penicillin used for various infections, including ear infections, sinusitis, urinary tract infections, and respiratory infections
Cephalosporins
- Cephalexin: Effective against many types of bacteria and commonly prescribed for skin and soft tissue infections, urinary tract infections, and respiratory tract infections
- Ceftriaxone: Used for more severe infections such as meningitis, pneumonia, and certain sexually transmitted infections
Macrolides
- Azithromycin: Used for respiratory tract infections, including bronchitis and pneumonia, as well as skin and soft tissue infections
- Clarithromycin: Effective against respiratory tract infections, skin and soft tissue infections, and certain gastrointestinal infections
Fluoroquinolones
- Ciprofloxacin: Used for urinary tract infections, respiratory tract infections, and certain types of gastrointestinal infections
- Levofloxacin: Effective against respiratory tract infections, urinary tract infections, and skin and soft tissue infections
Tetracyclines
Doxycycline: Used for a wide range of bacterial infections, including respiratory tract infections, skin infections, and certain sexually transmitted infections
Sulfonamides
Trimethoprim/Sulfamethoxazole (TMP/SMX): Effective against urinary tract infections, respiratory tract infections, and certain gastrointestinal infections
In some cases, bacterial infections may require intravenous antibiotics or a combination of different antibiotics for more severe or complicated infections. Healthcare professionals make treatment decisions based on individual circumstances, considering factors such as the type and location of infection, the overall health of the individual, and any known antibiotic resistance patterns.
What is antibiotic resistance?
Antibiotic and Antimicrobial resistance occurs when bacteria develop the ability to survive and grow in the presence of antibiotics that were once effective in killing or inhibiting their growth. It is a natural evolutionary process that bacteria undergo in response to the selective pressure imposed by the use of antibiotics. When bacteria are repeatedly exposed to antibiotics, either due to improper use, incomplete treatment, or overuse, they can adapt and develop mechanisms to resist the effects of these drugs.
The development of antibiotic resistance poses a significant challenge in the treatment of bacterial infections. It means that the antibiotics that were once effective in killing or controlling bacterial infections may no longer work against resistant bacteria. This can lead to persistent or recurrent infections, prolonged illness, increased healthcare costs, and a higher risk of complications.
There are several ways in which bacteria can become resistant to antibiotics:
- Genetic Mutations: Bacteria can acquire genetic mutations that enable them to withstand the effects of antibiotics. These mutations may alter the target sites of the antibiotics or enhance the bacteria’s ability to pump out or neutralize the drugs
- Horizontal Gene Transfer: Bacteria can transfer genetic material, including antibiotic resistance genes, to other bacteria. This can occur through mechanisms such as conjugation, transformation, or transduction, allowing the rapid spread of resistance genes among different bacterial species
The consequences of antibiotic resistance are far-reaching. It affects the effectiveness of common antibiotics and limits treatment options for bacterial infections. This has led to the emergence of multidrug-resistant bacteria, also known as superbugs, which are resistant to multiple classes of antibiotics. Infections caused by these superbugs can be difficult to treat and may require more potent, specialized antibiotics that are often associated with increased side effects and higher costs.
To combat antibiotic resistance, it is crucial to use antibiotics responsibly and judiciously. This includes following prescribed treatment regimens, completing the full course of antibiotics, avoiding the use of antibiotics for viral infections (e.g., common cold, flu), and preventing the overuse of antibiotics in agriculture and livestock production.
Summary
Bacterial infections are a prevalent health concern affecting various body systems. Recognizing the causes, types, symptoms, and available treatments for bacterial infections is crucial for prompt diagnosis and effective management. By practicing good hygiene, seeking timely medical care, and adhering to prescribed treatments, individuals can reduce the risk of bacterial infections, promote recovery, and safeguard overall health.
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.