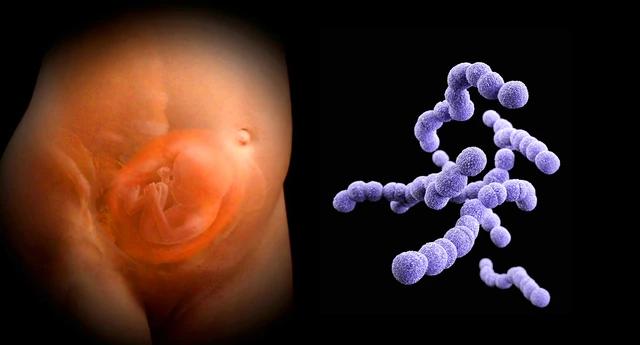
Group B Streptococcus (GBS), also known as Streptococcus agalactiae or Group B Strep is a common bacterium found in the gastrointestinal and genital tracts of healthy adults. While it is usually harmless in these individuals, GBS can pose a significant threat to newborns and individuals with certain underlying health conditions. Understanding the risks, symptoms, and prevention strategies associated with GBS is important in the safeguarding and well-being of both expectant mothers and their infants.
What is Group B Streptococcus?
Group B Streptococcus is a type of bacteria normally present in the human body in the intestines or lower genital tract. GBS is common and usually harmless, with many healthy adults carrying the bacteria without any adverse effects. However, in certain situations, such as during pregnancy or in people with compromised immune systems, GBS can become a serious health concern.
Prevalence and transmission
1 in 4 pregnant women are estimated to be carriers of GBS bacteria. The bacteria can be transmitted from the mother to the baby during childbirth, when the baby comes into contact with or swallows fluids containing the bacteria. GBS is not a sexually transmitted infection (STI) and is not spread through food or water.
Differences from Group A Streptococcus
Group B Streptococcus is distinct from Group A Streptococcus, the bacteria responsible for causing strep throat. These two streptococcal groups have different characteristics and disease manifestations.
Risks and complications of GBS infection
The risks and complications associated with GBS can vary depending on the individual’s age, health, and the specific stage of infection.
Risks for infants
Infants are more vulnerable to GBS infections, which can lead to severe and life-threatening complications. Newborns can develop early-onset GBS disease, typically within the first 6 days of life, or late-onset GBS disease, which can occur up to 3 months after birth. The most common GBS-related infections in infants include:
- Pneumonia
- Sepsis (bloodstream infection)
- Meningitis (inflammation of the membranes surrounding the brain and spinal cord)
Factors that increase an infant’s risk of developing GBS disease include:
- The mother’s GBS status during pregnancy
- Premature birth (before 37 weeks of gestation)
- Prolonged rupture of the mother’s membranes (water breaking) before delivery
- Maternal fever during labor
- A previous history of GBS-affected pregnancies
Risks for adults
While GBS infections are more common in newborns, adults can also be affected, particularly those with certain underlying health conditions or weakened immune systems. The most common GBS-related infections in adults include:
- Urinary tract infections
- Skin and soft tissue infections
- Pneumonia
- Bacteremia (bloodstream infection)
- Bone and joint infections
Individuals at increased risk of GBS disease as adults include:
- Adults aged 65 and above
- Individuals with chronic medical conditions, such as diabetes, liver disease, or HIV/AIDS
- Individuals with compromised immune systems
Symptoms of GBS infection
The symptoms of GBS infection can vary depending on the specific type of infection and the individual’s age.
Symptoms in infants
Infants with GBS disease may exhibit the following symptoms:
- Fever or low body temperature
- Difficulty feeding
- Lethargy or weakness
- Irritability or jitteriness
- Difficulty breathing
- Seizures
- Rash
Symptoms in adults
Adults with GBS infections may experience symptoms such as:
- Urinary tract infection symptoms
- Fever and chills
- Cough and shortness of breath (in cases of pneumonia)
- Swelling, warmth, or redness in the area of the infection
- Pain or stiffness in the affected area (in cases of bone or joint infections)
It is important to note that some adults may carry GBS without having any symptoms at all, making it crucial for pregnant women to have routine screening.
Screening and diagnosis
Routine screening for GBS during pregnancy is a crucial step in preventing the transmission of the bacteria to newborns.
Screening for pregnant women
The American College of Obstetricians and Gynecologists (ACOG) recommends that all pregnant women undergo GBS screening between weeks 36 and 37 of gestation. This involves taking a swab sample from the vagina and rectum, which is then sent for analysis.
If the test results indicate the presence of GBS, the healthcare provider will typically administer intravenous (IV) antibiotics during labor to help reduce the risk of the baby developing a GBS infection.
Diagnosing GBS infection
In cases where a GBS infection is suspected, additional tests to confirm the diagnosis include:
- Blood tests
- Spinal fluid analysis
- Urine tests
- Chest X-rays
Prompt diagnosis and appropriate treatment are vital, as GBS infections can quickly become life-threatening, particularly in newborns and individuals with weakened immune systems.
Prevention and management
Fortunately, there are several measures that can be taken to help prevent the transmission of GBS and manage the risks associated with the infection.
Preventing GBS transmission in newborns
The primary strategy for preventing GBS transmission from mother to baby during childbirth is the administration of intravenous antibiotics during labor, to reduce the risk of early-onset GBS disease in newborns.
In cases where a woman is allergic to penicillin or related antibiotics, clindamycin or vancomycin, may be used. However, the effectiveness of these drugs as an alternative is not as well-established, and the baby may require additional monitoring.
Preventing GBS infections in adults
Healthcare providers can take steps to reduce the risk of GBS-related complications in individuals with underlying medical conditions or weakened immune systems. These steps may include:
- Closely monitoring individuals at high risk
- Promptly treating any GBS-related infections with appropriate antibiotics
- Encouraging good hygiene and infection control practices
Managing GBS infections
When a GBS infection is suspected or diagnosed, prompt medical intervention is crucial to prevent the development of severe complications.
Treatment for infants
Infants are typically treated with intravenous antibiotics, which may be administered in the hospital setting. The duration and antibiotic regimen will depend on the severity and type of the infection.
Treatment for adults
Adults are also treated with antibiotics, either intravenously or orally, depending on the severity and location of the infection. In some cases, additional treatments, such as surgery, may be necessary for certain types of GBS-related infections.
Prognosis and recovery
The prognosis for individuals with GBS infections can vary depending on the severity of the infection, the individual’s overall health status, and the timeliness of the diagnosis and treatment.
Prognosis for infants
Most infants with GBS disease can make a full recovery, with prompt and appropriate treatment. However, GBS infections can lead to serious complications, such as permanent hearing loss, vision impairment, or even death, particularly in cases of early-onset disease.
Prognosis for adults
The prognosis for adults depends on the individual’s underlying health condition and the severity of the infection. With timely and effective treatment, many adults can recover from GBS-related infections without long-term consequences. However, in some people with weakened immune systems, GBS infections can be more severe and require extended treatment.
Ongoing research and future developments
While significant progress has been made in the understanding and management of GBS infections, ongoing research and development efforts are aimed at further improving prevention and treatment strategies.
Vaccine development
One of the key areas of research is the development of a GBS vaccine, which could help prevent GBS infections in both pregnant women and the general population. Several vaccines are currently in various stages of clinical trials, to provide a more comprehensive solution to the GBS challenge.
Conclusion
Group B Streptococcus is a common bacterium that poses a threat to newborns and individuals with certain underlying health conditions. By understanding the risks, symptoms, and prevention strategies associated with GBS, you and your healthcare provider can work together to safeguard your well-being.
Sources
- Group B strep disease – Symptoms & causes – Mayo Clinic
- About Group B Strep Disease – Group B Strep Disease – CDC
- Group B strep – NHS
- Group B Strep and Pregnancy – ACOG
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.