
In today’s world, chronic diseases have become increasingly common. The World Health Organization (WHO) states that people with a BMI greater than 25 have a higher risk of developing certain chronic diseases, such as type 2 diabetes, heart disease, kidney disease, non-alcoholic fatty liver disease, mobility issues and stroke. In the UK in 2007, it is estimated that being overweight, obesity and related morbidity costs the NHS £4.2 billion and these costs are predicted to reach £9.7 billion by 2050. Did you know that your body mass index (BMI) plays a critical role in the development of these conditions? In this blog post, we’ll explore what BMI means and how it is linked to various chronic diseases. We’ll also discuss effective ways to manage your BMI to reduce the risk of developing these debilitating illnesses.
Defining BMI
BMI stands for body mass index and is a widely used measurement to assess whether someone’s weight is healthy or not. It takes into account both height and weight, but it does not differentiate between muscle mass and fat mass. Studies have shown that having a higher BMI can increase the risk of chronic diseases such as cardiovascular disease, type 2 diabetes, and certain cancers. However, it’s important to remember that BMI is just one factor in assessing overall health status, and behaviour also plays a significant role in the development of these chronic diseases.
While some may argue that BMI doesn’t play a causal role in chronic disease development, studies have consistently shown an association between high BMI and increased risk for chronic diseases like cardiovascular mortality. Regardless of causality debates, we know that making efforts to maintain healthy BMIs through lifestyle changes can reduce overall risks associated with common non-communicable illnesses prevalent today – especially since obesity remains one of our biggest public health challenges globally.
What is BMI?
BMI stands for Body Mass Index, and it is a way to measure body fat based on height and weight. Understanding BMI is crucial for individuals who want to prevent or manage chronic diseases such as cardiovascular disease or type 2 diabetes. Research has shown that there is a causal role between high BMI levels and an increased risk of developing chronic diseases. In other words, having a higher BMI can lead to behaviours that increase the likelihood of developing these conditions.
Understanding your BMI is crucial for preventing chronic diseases like cardiovascular disease and type 2 diabetes. Knowing your own BMI level can help you take control of your health and make lifestyle changes if needed, leading to significant improvements in overall wellbeing.
Knowing your own BMI level is essential because it can help you take control of your health by making lifestyle changes if needed. Even small reductions in body weight have been associated with significant improvements in cardiovascular mortality and various other chronic diseases. Therefore, knowing your own BMI level can be the first step towards achieving long-term health goals, improving overall well-being, while reducing the risk of numerous medical issues down the line.
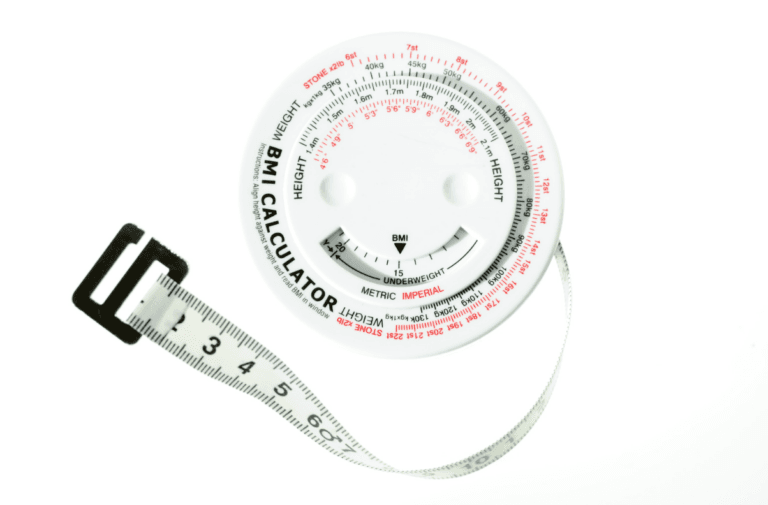
How is BMI calculated?
Calculating your BMI is a simple process that can be done at home. First, measure your weight in kilograms and your height in meters. Next, square the value of your height. Finally, divide your weight by the squared value of your height to get your BMI score. However, it’s important to note that different formulas are used for adults and children due to differences in body composition and growth patterns.
While calculating BMI can provide some insight into one’s overall health status, it should not be solely relied upon as an accurate indicator of an individual’s health risks or behaviour patterns. Factors such as muscle mass or bone density may affect the accuracy of calculated BMI scores. In addition, while there is evidence suggesting a causal role between high BMIs and chronic diseases like cardiovascular mortality, it’s important to remember that each person’s relationship with their own body goes beyond numbers on a scale or formula calculations.
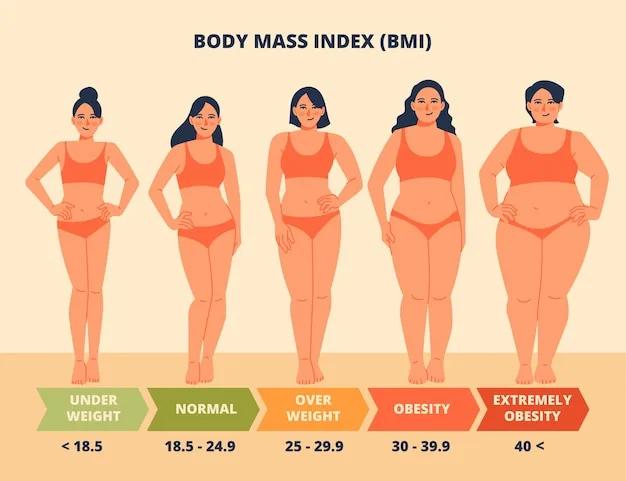
NHS guidelines on BMI values
A BMI calculation in the healthy weight range is between 18.5 to 24.9.
For Black, Asian and some other minority ethnic groups, the healthy weight range is 18.5 to 23.
For people of White heritage, a BMI:
- below 18.5 is underweight
- between 18.5 and 24.9 is healthy
- between 25 and 29.9 is overweight
- of 30 or over is obese
Black, Asian and some other minority ethnic groups have a higher risk of developing some long-term conditions such as type 2 diabetes with a lower BMI. People from these groups with a BMI of:
- 23 or more are at increased risk (overweight)
- 27.5 or more are at high risk (obese)
A person’s BMI is a useful indicator of their overall health, but it is not without limitations. For instance, it does not account for muscle mass or body composition and is not accurate for everyone, such as bodybuilders or pregnant women.
Waist-to-height ratio
You could have a healthy-looking BMI but still have more belly fat than is recommended for optimal health. It’s a simple calculation that involves dividing your waist circumference by your height. Measuring your waist-to-height ratio might be just what you need to determine whether or not you’re carrying excess tummy fat. We often forget the importance of checking our waist circumference measurements, but it’s a key aspect of assessing our overall health.
A large waist circumference is associated with an increased likelihood of developing type 2 diabetes, cardiovascular disease and other health problems Men are at higher risk of type 2 diabetes if they have a waist circumference of 94-102cm and are at very high risk if it is more than 102cm. Women are at higher risk if they have a waist circumference of 80-88cm and at very high risk if it is more than 88cm.
Facts on Obesity in the UK
In England, the prevalence of obesity is not spread equally. The prevalence of obesity varies with socioeconomic environment. The greatest rates of obesity are seen in the most deprived parts of the country. Obesity prevalence was lowest among adults living in the least deprived areas (20%) and highest in the most deprived areas (34%).
The proportion of men who were either overweight or obese was lowest in the least deprived quintile (64%) and highest in the most deprived quintiles (72% and 71% in the fourth and most deprived group, respectively). Data on adolescent and childhood obesity paints a similar picture.
A much greater difference was seen for women than for men. For women, the proportion who were either overweight or obese was 52% in the least and second least deprived quintiles, compared with 72% in the most deprived.
The UK compares poorly to other high-income countries and has one of the highest rates of obesity in Europe. Average adult obesity prevalence across the nine EU countries where comparable data is collected is 23%, compared to 28% in the UK.
The Link Between BMI and Chronic Diseases
Maintaining a healthy BMI is crucial in preventing chronic diseases such as diabetes, heart disease, and stroke. A high BMI puts extra pressure on the organs and can lead to inflammation in the body. This inflammation can contribute to the development of chronic diseases. It is essential to understand that losing even a small amount of weight through healthy lifestyle changes can make a significant impact on reducing your risk for chronic diseases.
Understanding Chronic Diseases
Chronic diseases are long-term health conditions that require ongoing medical attention and can significantly impact a person’s quality of life. They include diabetes, heart disease, cancer, and arthritis among many others. Chronic diseases develop slowly over time and may last for years or even a lifetime.
Several factors contribute to the development of chronic diseases such as high blood pressure, high cholesterol levels, smoking, poor diet choices like excess sugar intake or lack of fruits and vegetables in one’s diet; physical inactivity; family history/genetics; age; and gender among others. Maintaining a healthy weight is also crucial in preventing chronic diseases as a higher BMI (Body Mass Index) has been linked to an increased risk of developing these illnesses. Understandably this can be challenging at times, but making small changes over time can lead to better health outcomes for those living with chronic illness, or those who are at risk for developing them later on down the road.
How BMI Affects Chronic Diseases
BMI is a measure of body fat based on height and weight. It’s simple to calculate, but its implications for overall health are complex. A high BMI indicates a greater risk of chronic diseases such as diabetes, heart disease, and some types of cancer. Conversely, a low BMI can also increase the risk for certain chronic conditions.
Research has shown that maintaining a healthy BMI is crucial in reducing the chances of developing chronic diseases like hypertension and kidney disease. This means that individuals with high BMIs should consider making lifestyle changes such as exercise and healthier eating habits to reduce their risks. Additionally, those with low BMIs may need to work with healthcare professionals to ensure they’re getting enough nutrients and calories needed for optimal health, while avoiding malnutrition-related conditions like osteoporosis or fertility issues.
Examples of Chronic Diseases Linked to BMI
BMI and Diabetes Mellitus:
Type 2 diabetes is a chronic disease that affects millions of people worldwide. The obesity epidemic increasingly drives the rates of type 2 diabetes. Excess weight contributes to insulin resistance, making it harder for the body to regulate blood sugar levels effectively.
When the body carries excess weight, it can no longer efficiently use or produce insulin, the hormone that controls blood glucose levels. According to studies, even slight excess weight increases the risk of developing type 2 diabetes, and the risk increases exponentially, depending on the severity of obesity.
Obesity may trigger changes to the body’s metabolism that cause adipose tissue (fat) to release increased amounts of fatty acids, glycerol, hormones, pro-inflammatory cytokines and other factors that are involved in the development of insulin resistance. When insulin resistance is accompanied by dysfunction of pancreatic islet beta-cells (the cells that release insulin) it leads to failure to control blood glucose levels
BMI and Heart Disease:
A high BMI is a significant risk factor for heart disease, which is the leading cause of death worldwide. Excess weight forces the heart to work harder than it should, putting a strain on the cardiovascular system. This strain contributes to the development of heart disease. Studies also found that overweight individuals are more likely to have high blood pressure, high cholesterol levels, and triglycerides, all of which increase the risk of heart disease.
BMI and Cancer:
Obesity increases the risk of developing various types of cancers like breast cancer, colon cancer, endometrial cancer, and kidney cancer. High levels of body fat can impact the production of certain hormones that have been linked to cancer development. Maintaining a healthy BMI and incorporating physical activity can lower the risk of developing cancer.
BMI and Respiratory Disorders:
A high BMI can cause respiratory disorders like sleep apnea, asthma, and pulmonary embolism. Obese individuals are more likely to develop respiratory disorders than individuals with normal weight. Lifestyle modification and a healthy BMI can decrease the risk of developing respiratory disorders.
While these conditions are serious and can be challenging for patients and caregivers alike, understanding how BMI plays a role in them may help individuals take proactive steps towards maintaining their health. For instance, choosing healthy foods and regular exercise can help manage weight while also reducing risks associated with these diseases. Overall awareness about BMI’s impact on chronic illnesses may empower patients to make informed decisions about their lifestyle choices and work towards improving their quality of life despite battling these conditions daily.
Managing BMI to Reduce the Risk of Chronic Diseases
Maintaining a healthy BMI is essential in reducing the risk of chronic diseases. Studies have shown that individuals with a high BMI are more likely to develop conditions such as type-2 diabetes, heart disease and stroke. Understanding the role BMI plays in these illnesses can help patients take steps towards managing their weight and leading a healthier lifestyle.
Implementing simple lifestyle changes like exercising regularly and choosing a balanced diet can significantly improve your BMI. However, medical interventions may be necessary for some individuals struggling with obesity or other health conditions affecting their weight. It’s crucial to work closely with healthcare professionals who can guide effective ways to manage your BMI while considering any underlying health concerns you may have.
Lifestyle Changes to Improve BMI
While our genes influence our risk of obesity; the impact of their contribution can be modified by environmental factors such as our lifestyle habits. The key to managing BMI and reducing the risk of chronic diseases lies in lifestyle changes, weight management interventions and prioritising healthy dietary habits. Here are some tips to get started:
- Healthy Diet: Focus on nutrient-dense foods like fruits, vegetables, lean proteins, and whole grains. Limit processed foods and sugary drinks
- Regular Exercise Routine: Incorporate regular physical activity into your daily routine. This can include activities like walking, jogging, cycling or swimming
- Stress Management Techniques: Practice stress-reducing techniques such as meditation or yoga. Engage in activities you enjoy such as reading or hobbies to take your mind off things
Taking small steps towards a healthier lifestyle can make a big difference when it comes to improving BMI levels and overall health outcomes. Make these changes sustainable by finding ways to incorporate them into your daily life consistently over time.
Medical Interventions to Manage BMI
When it comes to managing BMI, there are a few medical interventions that healthcare professionals can prescribe or perform. These options include prescription medications for weight loss, bariatric surgery options, and hormone therapy treatments.
- Prescription Medications for Weight Loss: Certain medications can be prescribed to help patients lose weight by suppressing appetite or blocking the absorption of fat
- Bariatric Surgery Options: For patients with severe obesity and related health conditions, bariatric surgery may be recommended as an option to reduce BMI and improve overall health
- Hormone Therapy Treatments: In certain cases where hormonal imbalances contribute to excess weight gain, hormone therapy may be a viable treatment option
Patients need to discuss these medical interventions with their healthcare professionals to determine the best plan of action based on individual needs and goals.
Working with Healthcare Professionals
Regular Check-Ups and Monitoring Progression, ‘Ask Me Anything’ Sessions with Doctors and Nutritionists, and Support Groups: Finding Emotional Support from Peers in Similar Situations – are just some of the ways you can work with healthcare professionals to manage your chronic disease effectively. It’s crucial to have a supportive network around you as you navigate through your illness. Here are some insights on how working closely with healthcare professionals can help:
- Regular Check-Ups and follow up: Scheduling regular check-ups is essential for tracking progress and making necessary adjustments to treatment plans. Your clinician will monitor your BMI, blood pressure, cholesterol level etc., and assess any changes or improvements that need to be made
- ‘Ask Me Anything’ Sessions with Doctors and Nutritionists: One-on-one sessions enable patients to ask questions regarding their condition or lifestyle changes they should make. These sessions help patients understand their situation better while receiving personalised advice on managing their BMI
- Support Groups: Finding Emotional Support from Peers in Similar Situations: Joining support groups gives individuals an opportunity for emotional connection by sharing experiences in similar situations
Working alongside healthcare professionals helps ensure that you receive appropriate care tailored explicitly towards your needs. It allows patients insight into what sustains good health management practices going forward, while having a haven or community where one feels seen heard and understood.
Why BMI alone isn’t enough
Whilst BMI is an important indicator of health, it isn’t the only factor that healthcare professionals consider when assessing the risk of chronic diseases. Other factors that need to be taken into account include smoking, alcohol consumption, physical activity levels, and diet. To get a complete picture of your risk of chronic disease, it’s important to look at these factors as well as your BMI.
Conclusion
In conclusion, understanding the role that BMI plays in chronic diseases is crucial for maintaining good health. By monitoring your BMI and taking steps to maintain a healthy weight, you can reduce your risk of developing chronic diseases such as heart disease, diabetes, and certain types of cancer. Remember to consult with your healthcare provider if you have any concerns or questions about managing your weight and reducing your risk for chronic diseases.
Overall, it’s important to approach BMI management from a holistic perspective that includes regular physical activity and a balanced diet. Small lifestyle changes can make a big difference in preventing chronic diseases and improving overall health outcomes. With dedication and support from healthcare providers and loved ones, anyone can achieve their goals for optimal health.
Sources
- Adult obesity and type 2 diabetes PDF – GOV.UK
- Health Survey for England, 2019: Data tables – NHS
- Health Survey for England, 2021 part 1 – NHS
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.