Psoriasis is a chronic skin condition that affects millions of people worldwide. It causes red, scaly patches on the skin that can be itchy, painful, and sometimes embarrassing. While the exact cause of psoriasis remains unknown, researchers have made significant progress in understanding its connection to the immune system.
What is Psoriasis?
Psoriasis is a chronic skin condition that causes red, scaly patches on the skin. These patches, known as plaques, can be itchy, painful, and sometimes embarrassing for those affected. The condition results from an overactive immune system, which causes skin cells to multiply too quickly. This rapid cell growth leads to the buildup of thick, scaly patches on the skin’s surface.
The appearance of psoriasis can vary depending on skin colour. On lighter skin tones, the patches may appear pink or red with silvery-white scales. On darker skin tones, the patches can look purple or dark brown with grey scales. Psoriasis commonly affects areas such as the elbows, knees, scalp, and lower back, but it can appear anywhere on the body.
Different types of psoriasis
There are several distinct types of psoriasis, each with its own unique characteristics and signs. Understanding the different forms of psoriasis is useful as it can help individuals and healthcare providers tailor the most appropriate treatment.
Plaque psoriasis
Plaque psoriasis is the most common form of the condition, affecting up to 90% of individuals with psoriasis. It is characterised by the presence of well-defined, raised plaques that are often covered in a silvery-white scale. These plaques are typically found on the elbows, knees, lower back, and scalp, although they can appear anywhere on the body.
Guttate psoriasis
Guttate psoriasis is a less common form that typically appears in children and young adults. It is often triggered by a bacterial infection, such as streptococcal throat infection, and appears by the sudden appearance of small, drop-like lesions on the trunk, arms, and legs. These lesions are usually salmon-coloured and may clear up on their own without treatment.
Inverse psoriasis
Inverse psoriasis is a type that mainly affects the skin folds, such as the armpits, groin, and under the breasts. Unlike other forms of psoriasis, inverse psoriasis typically presents as smooth, red patches without the characteristic scaling. This type of psoriasis can be particularly challenging to manage due to the moisture and friction in these areas.
Pustular psoriasis
Pustular psoriasis is a rare and severe form of the condition that causes the development of pus-filled blisters, often on the hands and feet. These blisters can be extremely painful and may be accompanied by fever, chills, and other systemic symptoms.
Erythrodermic psoriasis
This type is characterised by a widespread, fiery red rash that can cover the majority of the body, often accompanied by intense itching, pain, and systemic symptoms. Erythrodermic psoriasis is a medical emergency and requires prompt treatment to prevent potentially life-threatening complications.
Nail psoriasis
While not a distinct type of psoriasis, it is important to note that the condition can also affect the nails, leading to a variety of changes, such as pitting, discolouration, and even nail detachment. Nail psoriasis can be challenging to treat and may be an indicator of more severe forms of the disease.
Symptoms of psoriasis
Psoriasis has the appearance of thick, scaly patches on the skin, often referred to as “plaques.” These plaques can vary in size, colour, and location, depending on the type of psoriasis. However, there are several other common symptoms that individuals with psoriasis may experience:
Skin discoloration and scaling
Discoloured, raised patches on the skin. These patches can range in colour from red to purple or brown, depending on the individual’s skin tone, and are often covered in a silvery-white scale.
Itching
Many people with psoriasis report experiencing intense itching, burning, or soreness in the affected areas.
Joint pain
Approximately one-third of individuals with psoriasis also develop a related condition called psoriatic arthritis, which can cause joint pain, swelling, and stiffness. This complication can significantly impact an individual’s quality of life and mobility.
Nail changes
Psoriasis can also affect the nails, leading to a variety of changes, such as pitting, discolouration, thickening, and even separation from the nail bed.
Systemic symptoms
In rare and severe cases, psoriasis can also cause systemic symptoms, such as fever, chills, and general malaise. This is particularly true for the generalized pustular and erythrodermic forms of the condition, which require immediate medical attention.
The immune system and psoriasis
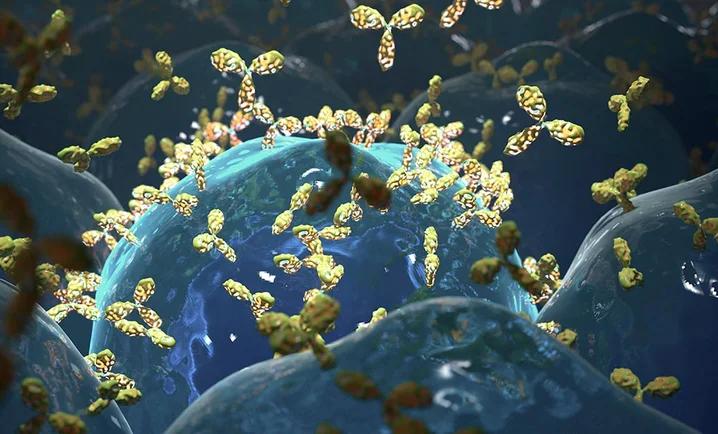
Psoriasis is a skin disease where the immune system mistakenly attacks healthy skin cells, causing rapid cell turnover and inflammation. The overactive immune response leads to the formation of thick, scaly plaques on the skin’s surface. While psoriasis shares many characteristics with autoimmune disorders such as the presence of T cells some experts argue that it doesn’t fully meet the criteria for classification as a true autoimmune condition.
This immune system dysfunction is thought to be a key driver of the condition but the exact causes of psoriasis are not fully understood. It is believed to be influenced by genetic and environmental factors too. Understanding the potential triggers and risk factors linked with the condition can help individuals take steps to manage symptoms and reduce the likelihood of flare-ups.
Genetics
Psoriasis is known to have a strong genetic link with studies indicating that individuals with a family history are more likely to develop it themselves. However, the inheritance pattern is not straightforward, and multiple genes are believed to be involved in the development of the disease.
Environmental triggers
While genetics play a significant role, certain environmental factors can also trigger or exacerbate psoriasis symptoms. These triggers can include:
- Infections, such as streptococcal throat infections
- Stress and emotional trauma
- Certain medications, including lithium and beta-blockers
- Skin injuries, such as cuts, scrapes, or severe sunburns
- Extreme weather conditions, particularly cold and dry environments
Underlying health conditions
Individuals with certain underlying health conditions may be at an increased risk of developing psoriasis. These conditions include obesity, type 2 diabetes, cardiovascular disease, hypertension (high blood pressure), rheumatoid arthritis, celiac disease, inflammatory bowel disease such as Crohn’s disease and mental health disorders, such as depression and anxiety.
Psoriasis treatment
There is no cure for psoriasis, but a wide range of treatment options are available to help manage the symptoms and improve the quality of life for those living with the condition. The specific treatment approach will depend on the type and severity of the psoriasis, as well as the individual’s overall health and preferences.
Topical treatments
Topical treatments, such as corticosteroid creams, vitamin D cream, and retinoids are applied directly to the affected areas of the skin and can help reduce inflammation, slow the growth of skin cells, and reduce symptoms.
Phototherapy
Healthcare providers may recommend phototherapy or light therapy, which involves exposing the affected areas of the skin to controlled amounts of ultraviolet (UV) light. This can help slow the rapid growth of skin cells and reduce inflammation.
Systemic medications
In cases where topical treatments and phototherapy are not effective, healthcare providers may prescribe systemic medications, such as oral or injectable immunosuppressants (methotrexate and cyclosporine) or biologic drugs (etanercept, infliximab). These medications work to balance the overactive immune system and can be particularly helpful for individuals with severe psoriasis.
Conclusion
Psoriasis, once considered solely a skin disorder, has shown strong links to the immune system, shedding light on its potential classification as an autoimmune disease. The influence of genetic factors and immune responses has an impact on the development and progression of psoriasis. This understanding has led to groundbreaking treatments that target specific immune pathways, offering hope to improve the lives of those affected by this chronic condition.
Sources
- Psoriasis: What It Is, Symptoms, Causes, Types & Treatment
- Psoriasis – Causes – NHS
- Psoriatic Disease Affects More Than Skin and Joints
- Psoriasis – Autoimmune Association
- Psoriatic Disease and the Immune System
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.