
Autoimmune diseases are complex conditions that affect millions worldwide. They can impact virtually any organ or system, causing a wide range of symptoms that can come and go unpredictably. From joint pain and fatigue to skin rashes and neurological issues, the effects of these diseases can be both physically and emotionally draining for those affected.
In this guide, we’ll look into autoimmune diseases, exploring their causes, symptoms, diagnosis, and the latest advancements.
What are autoimmune diseases?
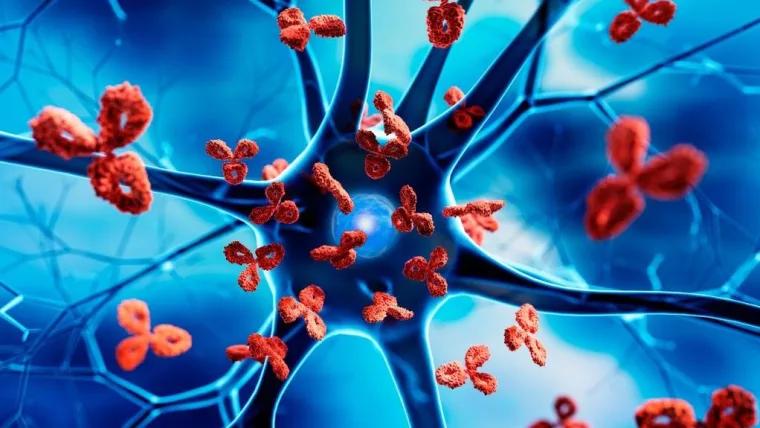
Autoimmune diseases are a diverse group of disorders characterised by the immune system’s attack on the body’s healthy tissues and cells. Unlike the typical immune response, which targets foreign invaders, the autoimmune process results in the body essentially turning against itself, causing inflammation, tissue damage, and a wide range of symptoms.
The exact reasons why the immune system fails in this way are not fully understood, but researchers believe that genetics and environmental factors play a crucial role. Certain genetics make individuals more susceptible to developing an autoimmune condition, while environmental triggers, such as infections, toxins, or even certain medications, can potentially activate the autoimmune response.
Common autoimmune diseases
Autoimmune diseases can affect virtually any body part, from the joints and muscles to the skin, digestive system, and nervous system. Some of the most well-known autoimmune disorders include:
- Rheumatoid arthritis: An inflammatory condition that primarily targets the joints, causing pain, swelling, and stiffness
- Lupus: A chronic, multisystem disorder that can affect various organs, including the skin, joints, and kidneys
- Multiple Sclerosis: A neurological condition in which the immune system attacks the protective myelin sheath surrounding nerve fibres, disrupting communication within the central nervous system
- Type 1 Diabetes: An autoimmune disease that destroys the insulin-producing cells in the pancreas, leading to an inability to regulate blood sugar levels
- Inflammatory bowel diseases (Crohn’s Disease and Ulcerative Colitis): Conditions characterised by chronic digestive tract inflammation
- Hashimoto’s Thyroiditis: An autoimmune disorder that targets the thyroid gland, leading to hypothyroidism and a range of hormonal imbalances
- Psoriasis: An autoimmune skin condition that causes the rapid buildup of skin cells, resulting in scaly, red patches
These are just a few examples of the diverse array of autoimmune diseases, each with its own unique set of symptoms and challenges.
Causes and risk factors
The underlying causes of autoimmune diseases are not yet fully understood, but researchers believe that a combination of genetic and environmental factors plays a crucial role in their development.
Genetic factors
Certain genetics can make individuals more susceptible to developing autoimmune disorders. Studies have shown that individuals with a family history of autoimmune diseases are at a higher risk of also developing these conditions. Specific genetic variations and mutations can affect the way the immune system functions, making it more prone to attacking the body’s own cells and tissues.
Environmental triggers
Environmental factors can also contribute to the development of autoimmune diseases. Exposure to certain infections, toxins, or even certain medications can potentially trigger the autoimmune response in individuals with a genetic predisposition. Additionally, factors such as stress, diet, and lifestyle choices may also influence the risk of developing these conditions.
Sex and age
Autoimmune diseases are more common in women than in men, with as many as 80% of cases occurring in females. Researchers believe that hormonal differences and the X chromosome, which contains a higher number of immune-related genes, may contribute to this gender difference.
Additionally, the onset of autoimmune diseases can vary widely, with some conditions typically appearing in childhood or adolescence, while others are more common in adulthood or the elderly.
Symptoms
The symptoms of autoimmune diseases can be diverse and wide-ranging, as they can affect virtually any part of the body. However, some common symptoms are often associated with these conditions:
- Fatigue and malaise: Autoimmune diseases can cause chronic fatigue, making it difficult for individuals to engage in daily activities
- Pain and inflammation: Many autoimmune disorders, such as rheumatoid arthritis and lupus, are characterised by joint pain, muscle aches, and widespread inflammation
- Skin problems: Conditions like psoriasis, dermatomyositis, and scleroderma can cause rashes, lesions, and other skin-related symptoms
- Digestive Issues: Autoimmune diseases affecting the gastrointestinal system, such as Crohn’s disease and ulcerative colitis, can lead to abdominal pain, diarrhoea, and digestive distress
- Neurological symptoms: Autoimmune disorders targeting the nervous system, like multiple sclerosis, can cause symptoms such as numbness, tingling, vision problems, and cognitive impairment
- Endocrine disruptions: Conditions like Hashimoto’s thyroiditis and type 1 diabetes can lead to hormonal imbalances and metabolic dysregulation
It’s important to note that the specific symptoms and their severity can vary greatly depending on the type of autoimmune disease and the individual’s unique response to the condition.
Diagnosis
Diagnosing autoimmune diseases can be a complex and challenging process, as many of these conditions share similar symptoms with other health issues. Healthcare providers often need to rely on a combination of medical history, physical examination, and laboratory tests to arrive at a proper diagnosis.
Medical history and physical exam
Initially, healthcare providers will gather a detailed medical history, the patient’s symptoms and any family history of autoimmune disorders. A physical examination may also reveal clues, such as joint swelling, skin rashes, or other physical signs of the condition.
Laboratory tests
- Laboratory tests play a crucial role in the diagnosis of autoimmune diseases. Some of the common tests used include:
- Antinuclear antibody test (ANA test): This test detects the presence of autoantibodies that target the body’s cells and tissues, which is a classic sign of many autoimmune conditions
- Erythrocyte Sedimentation Rate (ESR): This test measures the level of inflammation in the body, which can increase in autoimmune diseases
- Complete Blood Count (CBC): This test can help identify any abnormalities in the levels of different blood cells, which can indicate an underlying autoimmune disorder
- Specific Autoantibody Tests: Depending on the suspected autoimmune condition, healthcare providers may order tests for specific autoantibodies, such as rheumatoid factor for rheumatoid arthritis or thyroid peroxidase antibodies for Hashimoto’s thyroiditis
Treatment
While there is no cure for autoimmune diseases, a range of treatment options are available to help manage the symptoms, slow disease progression, and improve the overall quality of life for those affected.
Medications
The treatment approach for autoimmune diseases often involves the use of medications that aim to suppress the overactive immune system. These can include:
- Corticosteroids: These powerful anti-inflammatory drugs, such as prednisone, can help reduce inflammation and reduce symptoms
- Immunosuppressants: Medications like methotrexate, azathioprine, and mycophenolate mofetil can help suppress the immune system’s abnormal response
- Biologic Drugs: These targeted therapies, such as TNF-alpha inhibitors and interleukin blockers, can specifically target the underlying immune system failure
- Other medications: Depending on the specific condition, healthcare providers may also prescribe medications to address individual symptoms, such as pain relievers, antidepressants, or thyroid hormone replacement
Lifestyle changes
In addition to medication, lifestyle changes can also play a crucial role in managing autoimmune diseases. These may include:
- Dietary changes: Some research suggests that certain dietary factors, such as vitamin D, omega-3 fatty acids, and probiotics, may help modulate the immune system and reduce symptoms
- Exercise and physical therapy: Regular physical activity and targeted physical therapy can help improve joint function, muscle strength, and overall well-being
- Stress management: Techniques like meditation, yoga, and counselling can help individuals cope with the emotional and psychological aspects of living with an autoimmune disease
Conclusion
Autoimmune diseases are complex conditions that can have a profound impact on an individual’s physical, emotional, and social well-being. However, with a growing understanding of the disease, the development of new treatment options, and a focus on personalised care, there is reason for optimism for patients.
Sources
- Autoimmune Diseases: Types, Causes, Symptoms & Treatment
- National Institute of Environmental Health Sciences: Autoimmune Diseases
- Definition of autoimmune disease – NCI Dictionary of Cancer Terms – NCI
- Autoimmune disorders: MedlinePlus Medical Encyclopedia
- utoimmune Diseases – Autoimmune Disease Symptoms – MedlinePlus
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.







