Multiple Sclerosis
Get valuable insights into Multiple Sclerosis, including its causes, symptoms, prevention strategies, and treatment options, while also learning about how you can lower the cost of the medications used to treat Multiple Sclerosis.

MEDICAL INFORMATION
Multiple Sclerosis Key Facts
Related Medications
Multiple Sclerosis (MS) is a chronic autoimmune disease, where the immune system attacks the central nervous system (CNS). It is a complex and unpredictable condition, characterized by inflammation, demyelination, and damage to the protective covering of nerve fibers in the brain and spinal cord. MS is one of the most common neurological disorders, affecting millions of individuals worldwide. In this comprehensive article, we will delve into the various aspects of MS, including its causes, symptoms, diagnosis, treatment, and impact on daily life.
What is the definition of multiple sclerosis?
Multiple Sclerosis (MS) is a condition which is characterized by inflammation, demyelination, and damage to the protective covering of nerve fibers called myelin. MS is considered a neurodegenerative disorder in which the immune system mistakenly attacks the myelin, disrupting the normal transmission of nerve signals. This immune-mediated damage can also extend to the underlying nerve fibers themselves, leading to a variety of neurological symptoms. MS is a complex condition with a wide range of symptoms and disease courses, making it unique to each individual. It can present in various forms, including relapsing-remitting MS (RRMS), secondary progressive MS (SPMS), primary progressive MS (PPMS), and progressive-relapsing MS (PRMS). The exact cause of MS is unknown, but it is believed to involve a combination of genetic, environmental, and immunological factors. MS is a lifelong condition that requires ongoing management and care to alleviate symptoms, slow disease progression, and improve the quality of life for individuals living with the disease.
What are the causes and risk factors associated with multiple sclerosis?
The exact cause of Multiple Sclerosis (MS) is not fully understood. However, researchers believe that a combination of genetic, environmental, and immunological factors contribute to its development. Here are the causes and risk factors associated with MS:
Genetic Factors
MS is not directly inherited, but certain genes are thought to play a role in increasing the risk of developing the condition. Certain variations in genes related to the immune system, such as the HLA-DRB1 gene, have been identified as potential genetic risk factors for MS. However, having these genetic variations does not guarantee that an individual will develop the disease.
Environmental Factors
Environmental factors, including viral infections, have been implicated in the development of MS. Some viruses, such as Epstein-Barr virus (EBV), have been associated with an increased risk of MS. Additionally, factors like vitamin D deficiency, smoking, and exposure to certain chemicals may also contribute to the risk of developing MS.
Immune System Dysfunction
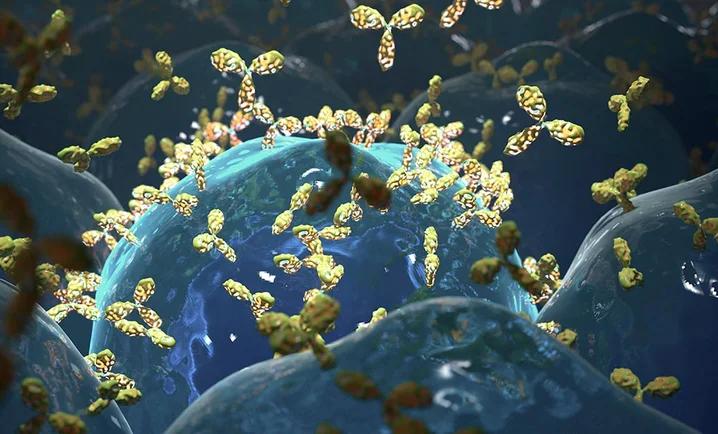
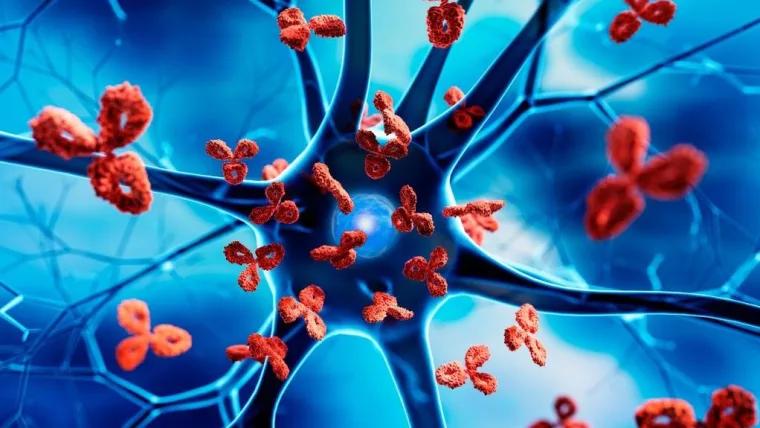
MS is considered an autoimmune disease, meaning that the immune system mistakenly attacks the body’s own tissues. In MS, the immune system targets the myelin, the protective covering of nerve fibers in the central nervous system. This immune response leads to inflammation, demyelination, and damage to the nerve fibers, resulting in the characteristic symptoms of MS.
Gender
MS is more common in women than in men. Women are about two to three times more likely to develop MS than men. The reason for this gender difference is not fully understood but may involve hormonal and genetic factors.
Age
MS can develop at any age, but it is most commonly diagnosed in young adults, typically between the ages of 20 and 40. However, MS can occur in children and older adults as well.
Family History
Having a first-degree relative (such as a parent or sibling) with MS increases the risk of developing the disease. However, the majority of individuals with MS do not have a family history of the condition.
It’s important to note that having one or more of these risk factors does not guarantee the development of MS. Many individuals with MS do not have any identifiable risk factors, and individuals without these risk factors can still develop the condition. The interplay between genetic, environmental, and immunological factors in the development of MS is complex and not fully understood. Ongoing research is focused on unraveling the specific causes and mechanisms underlying the disease.
What is the different types of multiple sclerosis?
Multiple Sclerosis (MS) can present in different forms, each with its own pattern of disease progression. The various types of MS include:
(RRMS) Relapsing-Remitting MS
This is the most common form of MS, affecting approximately 85% of individuals at the time of diagnosis. RRMS is characterized by unpredictable relapses or flare-ups of symptoms, followed by periods of partial or complete remission. During relapses, new symptoms may appear or existing symptoms may worsen. Remission periods are characterized by a reduction or disappearance of symptoms, although there may be residual deficits. Between relapses, there is usually a stable or improving condition.
Secondary Progressive MS (SPMS):
Some individuals with RRMS may eventually transition to SPMS. SPMS involves a gradual worsening of symptoms and a steady progression of disability, even without distinct relapses. In SPMS, there may still be occasional relapses or acute exacerbations, but they are typically less frequent and less pronounced compared to RRMS. SPMS may develop years or decades after the initial diagnosis of RRMS.
(PPMS) Primary Progressive MS
PPMS is less common, accounting for approximately 10-15% of MS cases. Unlike RRMS and SPMS, PPMS does not have distinct relapses and remissions. Instead, it involves a steady progression of symptoms from the onset, without significant periods of improvement. The progression of disability in PPMS can vary among individuals, with some experiencing a slow and gradual decline, while others may experience more rapid progression.
Progressive-Relapsing MS (PRMS)
PRMS is the least common form of MS, affecting a small percentage of individuals. It is characterized by a steady progression of symptoms from the onset, similar to PPMS. However, individuals with PRMS also experience occasional acute relapses or exacerbations, during which new symptoms may appear or existing symptoms may worsen. Following the relapse, there may be partial or incomplete recovery.
What is the pathophysiology of multiple sclerosis?
The pathophysiology of Multiple Sclerosis (MS) involves complex immune-mediated processes that result in inflammation, demyelination, and neurodegeneration within the central nervous system (CNS). The key components of MS pathophysiology are as follows:
MS Immune System Dysfunction
MS is considered an autoimmune disease, where the immune system mistakenly attacks components of the CNS, specifically the myelin sheath that surrounds nerve fibers. It is believed that certain environmental triggers activate the immune response in genetically susceptible individuals.
Inflammatory Response
In MS, immune cells, particularly T-cells, infiltrate the CNS and initiate an inflammatory response. These activated immune cells cross the blood-brain barrier and release pro-inflammatory cytokines and other molecules that promote inflammation in the CNS.
Demyelination
The immune response leads to the destruction of myelin, the protective covering of nerve fibers. Inflammatory cells, including macrophages and microglia, attack the myelin sheath, causing demyelination. This disrupts the normal conduction of nerve impulses and affects communication between neurons.
Formation of Lesions
Demyelination results in the formation of characteristic MS lesions, or plaques, which are areas of inflammation and myelin loss. These lesions can occur in various regions of the CNS, including the brain, spinal cord, and optic nerves.
Remyelination and Repair
In response to demyelination, the body attempts to repair the damage by initiating remyelination, a process in which oligodendrocytes (cells responsible for producing myelin) attempt to regenerate the myelin sheath. However, the remyelination process is often incomplete and may not fully restore normal nerve conduction.
Neurodegeneration
In addition to demyelination, MS also involves neurodegenerative processes. The loss of myelin, along with other factors such as chronic inflammation and oxidative stress, can lead to damage and loss of nerve cells (neurons) and their axons. This neurodegeneration contributes to the progressive accumulation of disability seen in many individuals with MS.
Reactive Gliosis and Scar Formation
Astrocytes, a type of glial cell, respond to the inflammatory environment by undergoing reactive gliosis. This process involves the activation and proliferation of astrocytes, which can lead to the formation of glial scars or plaques in the CNS. These scar formations can act as physical barriers that impede nerve regeneration and repair.
The exact triggers and mechanisms that initiate and perpetuate the immune response in MS are still unclear. It is believed to involve a combination of genetic susceptibility, environmental factors (such as viral infections), and dysregulation of the immune system. The immune-mediated inflammation, demyelination, and neurodegeneration collectively contribute to the wide range of symptoms and varying disease courses observed in individuals with MS. Ongoing research aims to further unravel the intricacies of MS pathophysiology and identify new therapeutic targets to prevent or slow down disease progression.
What are the signs and common symptoms of multiple sclerosis?
The specific symptoms experienced by individuals with MS can vary widely, depending on the location and extent of damage within the central nervous system (CNS). Some common signs and symptoms of MS include:
Fatigue
One of the most common and debilitating symptoms of MS is fatigue. It is characterized by a persistent lack of energy, exhaustion, and a decreased ability to carry out daily activities.
Motor Symptoms
MS can affect motor function and lead to various motor symptoms, including:
- Muscle Weakness: Weakness in the limbs, often asymmetrically, making it difficult to perform tasks requiring strength
- Spasticity: Increased muscle tone, stiffness, and involuntary muscle contractions, which can affect mobility and coordination
- Tremors: Involuntary shaking or trembling movements, particularly in the hands
Sensory Symptoms
MS can affect sensory perception and result in various sensory symptoms, such as:
- Numbness or Tingling: A sensation of pins and needles, numbness, or loss of sensation in the limbs, face, or other areas of the body
- Pain: Sharp, shooting, or burning pain, often in specific areas of the body, known as neuropathic pain
- Lhermitte’s Sign: Electric shock-like sensations that radiate down the spine and into the limbs, usually triggered by neck movements
Visual Disturbances
MS can affect vision and lead to visual symptoms, including:
- Optic Neuritis: Inflammation of the optic nerve, resulting in blurred vision, loss of vision in one eye, eye pain, or changes in color perception
- Double Vision (Diplopia): Seeing two images of a single object
Cognitive Changes
MS can impact cognitive function and lead to various cognitive symptoms, such as:
- Memory and Attention Problems: Difficulties with memory, concentration, information processing, and multitasking
- Problem-Solving and Decision-Making Challenges: Reduced ability to make decisions, solve problems, and plan complex tasks
- Slowed Thinking: Slower information processing speed, leading to delays in responding or processing new information
Emotional and Psychological Symptoms
MS can affect emotional well-being and lead to emotional and psychological symptoms, including
- Depression: Persistent feelings of sadness, hopelessness, or loss of interest in activities
- Anxiety: Excessive worry, fear, or unease
- Emotional Instability: Frequent mood swings, irritability, or emotional lability
Bladder and Bowel Dysfunction Symptoms
MS can impact bladder and bowel function, leading to symptoms such as
- Urinary Urgency and Frequency: A strong and sudden urge to urinate, along with increased frequency of urination
- Urinary Incontinence: Involuntary leakage of urine
- Constipation or Bowel Incontinence: Difficulty passing stools or loss of control over bowel movements
It’s important to note that not all individuals with MS will experience all of these symptoms, and the severity and combination of symptoms can vary among individuals. Additionally, MS symptoms can fluctuate over time, with periods of relapse and remission.
What are the stages of multiple sclerosis?
In Multiple Sclerosis (MS), the concept of distinct stages or phases of the disease is not commonly used in clinical practice. MS is a highly individualized condition, and the progression and course of the disease can vary widely among individuals. However, some healthcare professionals may refer to different stages of MS based on the accumulation of disability and progression of symptoms over time. These stages are not universally defined or agreed upon, but they can provide a general understanding of the disease’s progression. Here are a few commonly used stages or classifications of MS:
Clinically Isolated Syndrome (CIS)
CIS refers to the initial episode of neurological symptoms that lasts at least 24 hours and is caused by inflammation or demyelination in the CNS. CIS is the first clinical presentation that may indicate an increased risk of developing MS, but it does not meet the diagnostic criteria for MS itself.
Relapsing-Remitting MS (RRMS)
RRMS is characterized by episodes of relapse or flare-ups of neurological symptoms, followed by periods of partial or complete remission. Between relapses, there may be stability or some recovery. RRMS is the most common form of MS at the time of diagnosis.
Secondary Progressive MS (SPMS)
Some individuals with RRMS may eventually transition to SPMS. SPMS involves a gradual worsening of symptoms and a more steady progression of disability, even without distinct relapses. In this stage, there may still be occasional relapses or acute exacerbations, but they are typically less frequent and less pronounced than in RRMS.
Primary Progressive MS (PPMS)
PPMS is characterized by a steady progression of symptoms from the onset, without distinct relapses or remissions. Individuals with PPMS may experience a gradual decline in function and increased disability over time.
It’s important to note that these stages are not universally defined, and the course of MS can be highly variable among individuals. Some individuals may experience a relatively benign course with minimal disability progression, while others may have more aggressive disease progression leading to significant disability. Regular monitoring and communication with healthcare professionals are crucial to evaluate disease activity, track progression, and adjust treatment strategies as necessary.
How is multiple sclerosis diagnosed?
Diagnosing Multiple Sclerosis (MS) involves a comprehensive evaluation of an individual’s medical history, clinical presentation, and a series of diagnostic tests. There is no single test that can definitively diagnose MS, as the diagnosis is typically based on a combination of clinical findings and supportive evidence. The diagnostic process for MS commonly includes the following steps:
Medical History and Physical Examination
A healthcare professional or neurology specialist will review the individual’s medical history, including any previous neurological symptoms or episodes, family history of MS, and other relevant medical conditions. A thorough physical examination is conducted to assess neurological function, reflexes, coordination, and sensory perception.
Neurological Examination
A detailed neurological examination is performed to evaluate various functions, including vision, eye movements, muscle strength, coordination, reflexes, sensation, and balance. Neurological abnormalities or patterns of dysfunction may suggest the presence of MS.
Diagnostic Criteria
The healthcare professional will assess the individual’s symptoms and clinical findings to determine if they meet the diagnostic criteria for MS. The most widely used criteria for MS diagnosis are the McDonald criteria, which consider clinical and radiological evidence of the disease.
Magnetic Resonance Imaging (MRI)
MRI is a key diagnostic tool for MS. It allows visualization of the brain and spinal cord to detect characteristic MS lesions or plaques. These lesions appear as areas of inflammation and demyelination. Gadolinium, a contrast agent, may be administered to enhance the visibility of active lesions.
Lumbar Puncture (Spinal Tap)
A lumbar puncture may be performed to analyze the cerebrospinal fluid (CSF) obtained from the lower back. CSF analysis can help identify abnormalities, such as an increased level of specific immune cells or the presence of certain proteins (e.g., oligoclonal bands), which indicate inflammation and immune system activity in the CNS.
Evoked Potentials
Evoked potential tests measure the electrical responses of the brain or spinal cord to specific stimuli, such as visual, auditory, or sensory stimuli. These tests can help evaluate the conduction of nerve impulses and detect any delays or abnormalities, which may suggest demyelination in specific areas.
Differential Diagnosis
MS symptoms can overlap with those of other neurological conditions. The healthcare professional will consider and rule out other possible causes of symptoms, such as infections, vitamin deficiencies, structural abnormalities, or other autoimmune disorders.
Antibody Test
A test for MS that examines kappa immunoglobulin free light chains in cerebrospinal fluid.
How is multiple sclerosis prevented?
Currently, there is no known way to prevent the development of Multiple Sclerosis (MS). The exact cause of MS is not fully understood, and it is believed to result from a combination of genetic, environmental, and immunological factors. While prevention is not possible, there are some strategies that may help reduce the risk of developing MS or potentially delay its onset:
- Vitamin D: Adequate levels of vitamin D have been associated with a lower risk of developing MS. Spending time outdoors in sunlight, consuming foods rich in vitamin D (such as fatty fish, fortified dairy products, and egg yolks), or taking vitamin D supplements may be beneficial. However, further research is needed to fully understand the role of vitamin D in MS prevention
- Healthy Lifestyle: Maintaining a healthy lifestyle, including regular exercise, a balanced diet, and managing stress, may contribute to overall well-being and potentially reduce the risk of developing MS. While these lifestyle factors may not directly prevent MS, they can support overall health and potentially have a positive impact on immune function
- Avoidance of Smoking: Smoking has been associated with an increased risk of developing MS and can potentially worsen the disease course in individuals who already have MS. Quitting smoking or avoiding exposure to secondhand smoke is important for general health and may be beneficial for those at risk of or living with MS
- Minimizing Environmental Risk Factors: While specific environmental factors associated with MS development are not fully understood, some studies suggest that certain factors, such as viral infections (particularly Epstein-Barr virus), low exposure to sunlight, and exposure to certain chemicals, may influence the risk of developing MS. Minimizing exposure to potential risk factors, where possible, may be beneficial. However, it’s important to note that more research is needed to establish definitive links between environmental factors and MS risk
It’s crucial to emphasize that these preventive strategies are based on current knowledge and research, and their effectiveness in preventing MS is not fully established. MS is a complex disease with multifactorial causes, and individual risk factors and susceptibility can vary. While prevention may not be possible, early diagnosis, appropriate treatment, and management can help individuals with MS lead fulfilling lives and minimize the impact of the disease on their well-being. Regular check-ups, communication with healthcare professionals, and adherence to treatment plans are essential for those living with MS.
What are the treatment and management options for multiple sclerosis?
The treatment and management of Multiple Sclerosis (MS) aim to alleviate symptoms, modify the course of the disease, manage relapses, and improve the quality of life for individuals living with MS. The approach to treatment and management may vary depending on the type and severity of MS, as well as individual needs and preferences. Here are some common treatment and management options for MS:
Disease-Modifying Therapies (DMTs)
DMTs are medications used to modify the course of MS, reduce the frequency and severity of relapses, and slow down disease progression. There are various types of DMTs available, including injectable medications (interferons, glatiramer acetate), oral medications (fingolimod, dimethyl fumarate), and infusion therapies (natalizumab, ocrelizumab). The choice of DMT depends on factors such as disease activity, individual characteristics, and potential side effects. Regular monitoring is typically required to assess treatment effectiveness and adjust therapy as needed.
Symptomatic Treatments
Symptomatic treatments aim to manage specific symptoms associated with MS. These may include medications or therapies to alleviate fatigue, muscle spasticity, pain, bladder and bowel dysfunction, sexual dysfunction, cognitive impairment, and depression or anxiety. Symptomatic treatments are tailored to individual needs and may involve a multidisciplinary approach, including medications, physical therapy, occupational therapy, speech therapy, and psychological support.
Rehabilitation Therapies
Rehabilitation therapies play a crucial role in managing MS symptoms and improving functional abilities. Physical therapy focuses on improving mobility, strength, balance, and coordination. Occupational therapy helps individuals maintain independence in daily activities and addresses issues related to work, home modifications, and assistive devices. Speech therapy can assist with communication difficulties, swallowing difficulties, and cognitive impairments. Rehabilitation programs are designed based on individual needs and may include exercises, mobility aids, adaptive techniques, and strategies to enhance quality of life.
Healthy Lifestyle
Adopting a healthy lifestyle can support overall well-being and may have a positive impact on MS management. Regular exercise, tailored to individual abilities, can help improve strength, endurance, and mood. A balanced diet, rich in fruits, vegetables, whole grains, and lean proteins, is recommended. Managing stress through relaxation techniques, mindfulness, and stress-reducing activities can also be beneficial.
Emotional Support and Psychological Care
MS can have a significant emotional and psychological impact. Seeking emotional support from family, friends, and support groups can provide comfort and understanding. Mental health professionals, such as psychologists or counselors, can offer therapy and support to address anxiety, depression, and coping strategies.
Regular Monitoring and Disease Management
Regular check-ups with healthcare professionals, particularly neurologists or MS specialists, are essential for monitoring disease activity, adjusting treatment plans, and addressing emerging issues. Monitoring may involve clinical assessments, MRI scans, blood tests, and evaluations of treatment effectiveness.
It’s important for individuals with MS to work closely with healthcare professionals to develop an individualized treatment and management plan that addresses their specific needs and goals. Open communication, adherence to treatment plans, and proactive self-care can play a crucial role in optimizing overall well-being and managing the challenges associated with MS.
What medications are used in multiple sclerosis?
Interferon beta medications
- Interferon beta-1a (Avonex, Rebif, Plegridy)
- Interferon beta-1b (Betaseron, Extavia)
Glatiramer acetate (Copaxone, Glatopa)
Teriflunomide (Aubagio)
Dimethyl fumarate (Tecfidera)
Fingolimod (Gilenya)
Siponimod (Mayzent)
Natalizumab (Tysabri)
Ocrelizumab (Ocrevus)
Alemtuzumab (Lemtrada)
Mitoxantrone (Novantrone)
used in certain cases due to potential side effects and risks
What are the complications of multiple sclerosis?
Multiple Sclerosis (MS) can lead to various complications. The specific complications experienced by individuals with MS can vary widely depending on the severity of the disease and the areas of the central nervous system (CNS) affected. Here are some common complications associated with MS:
Physical Disability
MS can cause significant physical disability, particularly as the disease progresses. Motor symptoms such as muscle weakness, spasticity, balance problems, and coordination difficulties can impact mobility and activities of daily living. Some individuals may require assistive devices such as canes, walkers, or wheelchairs to aid with mobility.
MS Fatigue
Fatigue is a common and often debilitating symptom of MS. It can significantly impact daily activities, work, and quality of life. Fatigue in MS is often unrelated to the level of physical activity and may require energy conservation strategies, lifestyle modifications, and the use of medication to manage.
Bladder and Bowel Dysfunction
MS can affect the normal functioning of the bladder and bowel. Individuals may experience urinary urgency, frequency, hesitancy, or incontinence. Bowel dysfunction may manifest as constipation, diarrhea, or loss of bowel control. These symptoms can be managed through medications, dietary modifications, fluid management, and bowel training programs.
Sensory Disturbances
Sensory symptoms such as numbness, tingling, or pain can occur in MS. These sensory disturbances, also known as dysesthesias, can affect different parts of the body and impact daily activities and comfort.
Spasticity and Muscle Contractures
Spasticity, characterized by increased muscle tone and stiffness, can lead to muscle tightness and contractures. Contractures occur when muscles and tendons shorten and become rigid, limiting joint mobility. Physical therapy, stretching exercises, and medications can help manage spasticity and prevent contractures.
Cognitive Impairment
MS can affect cognitive function, including memory, attention, information processing, and problem-solving abilities. Cognitive impairments can impact work, social interactions, and overall quality of life. Strategies such as cognitive rehabilitation, compensatory techniques, and lifestyle modifications can help manage cognitive difficulties.
Emotional and Psychological Challenges
MS can have a significant impact on mental health and emotional well-being. Depression, anxiety, mood swings, and emotional lability are common in individuals with MS. Seeking support from mental health professionals, support groups, and maintaining a strong social network can help individuals cope with these challenges.
Sexual Dysfunction
MS can affect sexual function and lead to difficulties such as reduced libido, erectile dysfunction in males, and decreased vaginal lubrication in females. Open communication with healthcare professionals and the exploration of appropriate interventions can help manage these issues.
Respiratory Complications
In advanced stages of MS, respiratory muscles can become weak, leading to breathing difficulties and an increased risk of respiratory infections. Regular monitoring of respiratory function and interventions such as breathing exercises and assisted ventilation may be necessary.
Osteoporosis and Fractures
Individuals with MS are at an increased risk of developing osteoporosis due to factors such as reduced mobility, decreased weight-bearing activity, vitamin D deficiency, and the long-term use of corticosteroids. Preventive measures such as regular weight-bearing exercise, vitamin D supplementation, and medication interventions can help maintain bone health.
Promising research and future direction of multiple sclerosis
Multiple Sclerosis (MS) research is an active and rapidly evolving field. There are ongoing efforts to advance our understanding of the disease, develop more effective treatments, and improve the quality of life for individuals living with MS. Some promising areas of research and future directions in MS include:
- Disease-Modifying Therapies (DMTs): The development of new and more targeted DMTs continues to be a focus of research. Scientists are exploring novel mechanisms of action, identifying new drug targets, and investigating combination therapies to improve treatment outcomes and reduce disease activity
- Remyelination and Neuroprotection: Researchers are investigating strategies to promote remyelination, the process of restoring damaged myelin in the central nervous system. Various approaches, including the use of stem cells, remyelinating agents, and modulators of myelin repair processes, are being explored to enhance remyelination and protect nerve cells from damage
- Personalized Medicine: There is a growing interest in personalized medicine approaches for MS. Research aims to identify biomarkers and genetic factors that can predict disease progression, treatment response, and individualized treatment plans. This could help tailor therapies to each person’s specific needs, optimizing treatment outcomes
- Repair and Regeneration: Scientists are exploring strategies to promote repair and regeneration of damaged nerve cells and axons in MS. This includes studying the use of stem cells, neuroprotective agents, and growth factors to stimulate nerve cell regeneration and improve neurological function
- Symptom Management: Research is focused on developing more targeted and effective interventions for managing MS symptoms such as fatigue, spasticity, pain, and cognitive impairment. Non-pharmacological approaches, including neuromodulation techniques, rehabilitation strategies, and lifestyle interventions, are being investigated to enhance symptom management and improve quality of life
- Gut Microbiome and Environmental Factors: The role of the gut microbiome and environmental factors in MS development and progression is an area of active research. Scientists are exploring the interaction between gut bacteria and the immune system, investigating the impact of diet and environmental factors on MS risk and disease activity, and studying the potential of microbiome-based therapies for MS
- Advanced Imaging Techniques: Improvements in imaging technologies, such as advanced MRI techniques and molecular imaging, are enabling more precise visualization and characterization of MS lesions and disease activity. These techniques aid in earlier and more accurate diagnosis, monitoring treatment response, and understanding disease mechanisms
- Patient-Reported Outcomes and Quality of Life: Research is focused on understanding the impact of MS on individuals’ quality of life and developing interventions to address the physical, emotional, and social aspects of living with the disease. Patient-reported outcomes and patient-centered research are being emphasized to ensure that research outcomes align with the priorities and needs of individuals with MS
These are just a few examples of the many areas of research and future directions in MS. The ultimate goal is to better understand the underlying mechanisms of MS, develop more effective therapies, and improve the overall management and well-being of individuals living with the condition. Continued research efforts and collaboration among scientists, clinicians, and individuals with MS are crucial in advancing our knowledge and improving outcomes for this complex neurological disorder.
What multiple sclerosis support organisations are there available to support me in the UK?
- Multiple Sclerosis Society (MS Society): The MS Society is the largest UK charity organization dedicated to supporting individuals with MS. They provide a wide range of services, including information resources, support groups, helplines, grants for equipment and respite care, and research funding. They also offer a comprehensive website and an online community for connecting with others
- MS Trust: The MS Trust is a UK charity that offers information, resources, and support for individuals with MS and their families. They provide publications, webinars, a helpline, online forums, and educational materials. They also support healthcare professionals in delivering high-quality MS care
- Shift: Shift is a social network for young people living with MS. They provide an online community, information resources, and opportunities to connect with others through their website and social media platforms. They also offer a buddy system to connect newly diagnosed individuals with experienced MSers
- MS-UK: MS-UK is a national charity that provides information, support, and services to individuals affected by MS. They offer a helpline, counseling services, wellness programs, and educational resources. They also facilitate opportunities for peer support and social connections
- Overcoming Multiple Sclerosis (OMS): OMS is a nonprofit organization that focuses on promoting a holistic approach to managing MS through diet, exercise, and lifestyle modifications. They provide resources, educational materials, and support for individuals interested in adopting the OMS Recovery Program
What multiple sclerosis support organisations are there available to support me in the US?
- National Multiple Sclerosis Society (NMSS): The National MS Society is the largest nonprofit organization in the US dedicated to supporting individuals with MS. They provide a wide range of services, including information resources, support groups, financial assistance programs, advocacy efforts, and research funding. They also offer educational programs, wellness initiatives, and connections to local chapters
- Multiple Sclerosis Association of America (MSAA): The MSAA is a national nonprofit organization that provides support and resources for individuals with MS and their families. They offer a helpline, educational materials, cooling equipment distribution, MRI assistance programs, and a mobile phone app for managing MS symptoms. They also provide wellness programs and educational events
- Can Do Multiple Sclerosis: Can Do MS is a nonprofit organization that focuses on empowering individuals with MS to transform and improve their lives through comprehensive health and wellness education programs. They offer in-person and online programs that address various aspects of living with MS, including physical, emotional, and cognitive well-being
- Multiple Sclerosis Foundation (MSF): The MSF is a national nonprofit organization that provides support, educational programs, and direct services to individuals affected by MS. They offer assistance with medication costs, cooling equipment distribution, a helpline, educational resources, and wellness programs. They also provide support for caregivers and family members
- Multiple Sclerosis Research Institute (MSRI): The MSRI is a nonprofit organization that focuses on accelerating MS research to find improved treatments and a cure for the disease. They provide research funding, educational resources, and support for advancements in MS research
Summary
Multiple Sclerosis is a complex neurological condition that requires a multidimensional approach to diagnosis, treatment, and management. With ongoing research and advancements in care, individuals with MS can achieve a good quality of life and receive the support needed to navigate the challenges associated with the condition.
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.