In today’s society, there is an increasing emphasis on maintaining a healthy weight and body composition. One commonly used screening tool to assess weight-related health problems is the Body Mass Index (BMI). However, medical experts and researchers are questioning the accuracy and effectiveness of using BMI as the sole indicator of health. This article aims to delve into the limitations of BMI and explore why it may not always provide an accurate representation of an individual’s health status.
The origins and purpose of BMI
The concept of BMI can be traced back to Adolphe Quetelet, a Belgian mathematician who developed the formula in 1832. Initially, BMI was intended to describe the general population. rather than assess individual health. It gained popularity in the mid-20th century with actuaries who used it to determine risk and life insurance rates. Over time, certain BMI ranges were used as a predictor of increased risks of diseases and mortality, leading to the establishment of thresholds for categorizing individuals as “healthy” or “at-risk.”
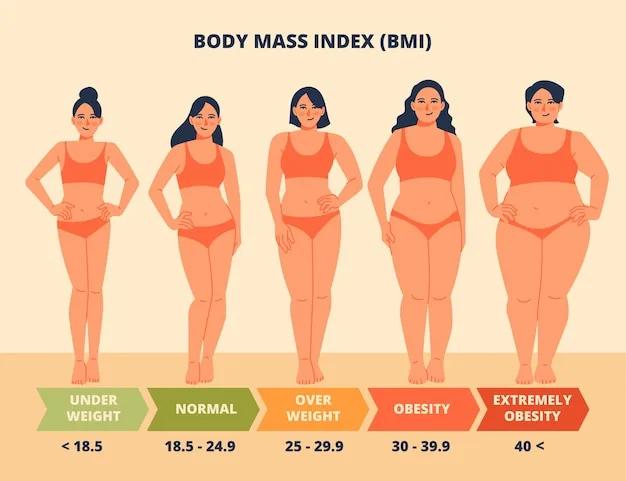
Understanding BMI calculation
BMI is calculated by dividing an individual’s body weight in kilograms by their height in meters squared. The resulting number is then interpreted within predefined ranges. For example, a BMI below 18.5 is considered underweight, while a BMI between 25 and 29.9 is classified as overweight. A BMI of 30 or above indicates obesity. However, it is crucial to remember that BMI does not provide a comprehensive picture of an individual’s health.
Limitations of BMI
1. Race and ethnicity
One of the significant limitations of BMI is its failure to account for biological and genetic differences among various racial and ethnic groups. Recent research highlights that weight, muscle mass, and disease risk vary across different populations. For instance, Asian or Middle Eastern individuals may be at higher risk for metabolic diseases like diabetes, even with a lower BMI compared to those of European descent. Employing a universal BMI cutoff may result in missed diagnoses and inadequate preventive care for these high-risk groups.
2. Muscle mass and athleticism
BMI does not differentiate between fat mass and lean muscle mass. Individuals with a higher percentage of lean muscle mass, such as athletes, may have a higher BMI, even though they possess excellent overall health. This discrepancy can lead to misclassification and potential misconceptions about an individual’s measure of health.
3. Weight distribution and waist circumference
BMI fails to consider weight distribution and waist circumference, which are crucial factors in determining health risks. People with a higher waist circumference, carrying excess fat distribution around the abdomen, are at a greater risk of metabolic and cardiovascular diseases compared to someone who carries weight in their lower body (pear-shaped). This oversight further challenges the accuracy of BMI as a measure of health.
Two individuals with the same BMI may have significantly different health profiles due to variations in weight distribution.
4. Age-related considerations
As individuals age, changes in body composition occur. Older adults tend to have more body fat and less muscle mass, which can impact BMI interpretation. Studies suggest that higher BMIs in older adults may offer protective benefits against certain diseases and premature death. Therefore, using a universal BMI cutoff for all age groups may not accurately reflect health risks.
5. Personal medical history
Each person’s medical history is unique and plays a significant role in determining their health risks. Individuals with a family history of specific diseases or preexisting conditions may need more individualized assessments beyond BMI.
6. Lifestyle factors
Lifestyle factors, such as diet, exercise, stress levels, and sleep patterns, can greatly impact health outcomes. While BMI does not account for these factors, they are essential considerations in determining an individual’s overall health.
The role of BMI in health assessment
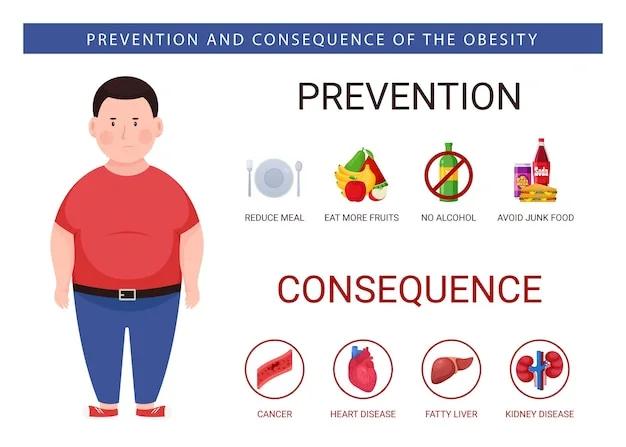
While BMI is not without its limitations, it still plays a role in assessing health risks when considered in conjunction with other factors. A high BMI is associated with an increased probability of developing various health conditions, such as diabetes, cardiovascular disease, and certain types of cancer. However, it is important to remember that BMI alone cannot provide a definitive diagnosis or predict an individual’s future health outcomes.
Additional indicators of health
To obtain a more comprehensive evaluation of an individual’s health, healthcare professionals consider multiple factors beyond BMI. These include:
- Blood pressure: A crucial indicator of cardiovascular health and risk. High blood pressure is a significant risk factor for heart disease
- Blood sugar levels: Screening for type 2 diabetes and pre-diabetes
- Cholesterol levels: Assessing the balance between LDL (bad) and HDL (good) cholesterol. Elevated cholesterol levels, particularly high levels of LDL (bad) cholesterol, increase the risk of heart disease and stroke
- Resting heart rate: A high resting heart rate may indicate increased risk for heart disease
- Inflammation markers: Chronic inflammation is linked to several chronic diseases, including cancer, diabetes, and cardiovascular diseases. Evaluating inflammation markers alongside BMI can provide a more comprehensive understanding of an individual’s health status
- Lean muscle mass versus fat mass: Assessing lean muscle mass, rather than just overall weight, provides insight into an individual’s body composition. Higher levels of lean muscle mass are associated with improved metabolic health and reduced risk of obesity-related conditions
- Waist circumference: Excess body fat around the abdominal area is linked to metabolic and cardiovascular diseases. Visceral fat which is fat stored deep in the belly, around the organs is associated with a number of health consequences
Moving beyond BMI
While BMI continues to be a useful tool for population-level health assessments, it should not be the sole determinant of an individual’s health status. Healthcare providers should consider a person’s unique characteristics, such as race, ethnicity, muscle mass, weight distribution, and age when evaluating a person’s health risks. Exploring alternative methods, like bioimpedance analysis, which provides a more accurate assessment of body fat percentage, can further enhance health evaluations.
Conclusion
BMI has served as a valuable tool in assessing weight-related health risks, but its limitations should be acknowledged. The one-size-fits-all approach of BMI fails to consider the diverse factors that contribute to an individual’s overall health. While a high BMI may indicate an increased probability of certain health conditions, it does not guarantee poor health or disease development. Healthcare professionals must consider multiple indicators, alongside BMI, to provide a comprehensive evaluation of an individual’s health status. By moving beyond BMI and adopting a more holistic approach, we can better understand and address the complexities of individual health.
Sources
- The unethical use of BMI in contemporary general practice – PMC
- Is BMI an Accurate Measure of Health? – Cleveland Clinic
- Body mass index (BMI) – Better Health Channel
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.