Urinary Incontinence Treatments
* Includes Free Private Prescription & Consultation.
† Applies to UK only.

START YOUR TREATMENT TODAY
Available Treatments for Urinary Incontinence
SAFE PRESCRIBING
Get Started With the Right Treatment for You
MEDICAL INFORMATION
Urinary Incontinence Key Facts
Urinary Incontinence is the unintentional passing of urine. It is more common in women and the elderly. Urinary Incontinence can be distressing and can impact on an individuals quality of life and mental well-being. There are various types, such as stress, urge, overflow, functional, mixed, reflex, and total incontinence, each with its own challenges.
Here, we will take a closer look at its causes, symptoms, diagnosis, management strategies and treatment options, as well as strategies for managing daily life, when living with Urinary Incontinence.
Understanding Urinary Incontinence
To manage the condition effectively, we need to understand the various types of Urinary Incontinence:
- Stress Incontinence (stress Urinary Incontinence):
- This occurs when physical activities such as coughing, sneezing, or exercise put pressure on the bladder, causing involuntary urine leakage
- Common in women, especially those who have experienced childbirth or menopause
- Management includes pelvic floor exercises and lifestyle modifications
- Urge Incontinence:
- Symptoms include a sudden, intense urge to urinate followed by urine leakage, with little warning
- Associated with conditions such as urinary tract infections or neurological disorders, which affect the bladder’s ability to hold urine
- Treatment may include bladder training, medication, or nerve stimulation techniques to help improve bladder control
- Overflow Incontinence:
- Caused by the bladder’s inability to empty completely, causing constant or frequent dribbling of urine
- Often caused by an obstruction in the bladder or urethra, or nerve damage, which can cause bladder problems
- Catheterization or surgery may be necessary
- Total Incontinence:
- Continuous urine leakage or frequent uncontrolled urination
- Caused by abnormalities in anatomy or damage to the urinary system
- Management includes surgical interventions or special containment devices
- Mixed incontinence:
- When you may have both urge and stress incontinence symptoms
By understanding which type of incontinence a person has, healthcare providers can tailor treatment strategies to improve bladder control and enhance quality of life.
Causes of Urinary Incontinence
The causes of Urinary Incontinence range from physiological to lifestyle:
- Age-related changes: Muscles supporting bladder control may weaken, and nerves that signal the need to urinate may not work as well as we age. This can cause the involuntary leakage of urine
- Pregnancy and childbirth place extra pressure on the bladder and pelvic floor muscles, potentially causing stress incontinence. Childbirth can lead to a dropped (prolapse) pelvic floor. With prolapse, the bladder, uterus, rectum or small intestine can get pushed down into the vagina
- A decline in estrogen during menopause can weaken the urinary tract muscles
- Excess weight and obesity increases pressure on the bladder, and may lead to stress incontinence
- Family history may play a role in predisposing individuals to Urinary Incontinence
- Underlying medical conditions, such as multiple sclerosis, diabetes, an enlarged prostate gland and urinary tract infections (UTIs) can impair bladder function
- Certain medications, such as diuretics, sedatives, and muscle relaxants, may increase the risk of Urinary Incontinence
- Alcohol, caffeine, and certain foods can irritate the bladder, making the symptoms of Urinary Incontinence worse
- Neural and structural damage to the bladder, sphincters, supporting structures, or pelvic floor can result in Urinary Incontinence
- Men who have had prostate surgery may develop stress incontinence
Addressing underlying causes is critical when receiving medical advice and treatment for Urinary Incontinence.
Symptoms and diagnosis
Diagnosis includes:
- Initial consultation to gather information about your symptoms and medical history
- Physical exam, including a stress test, where you are asked to perform activities that typically trigger urine leakage
- Diagnostic tests such as:
- Urinalysis, to check for signs of infection
- A record of your bladder activity
- Measurements of the amount of urine left in the bladder after urination
- Urodynamic testing, to test how well the bladder, sphincter muscles, and urethra are storing and releasing urine
- Cystoscopy
- Pelvic ultrasound, to check for abnormalities
These tests help to rule out other conditions that may cause Urinary Incontinence, such as urinary retention, which can lead to overflow incontinence.
Managing and treating Urinary Incontinence
Management of Urinary Incontinence involves non-invasive strategies to surgical interventions:
Lifestyle modifications and behavioural therapies:
- Maintaining a healthy weight to reduce pressure on the bladder
- Managing fluid intake and reducing bladder irritants like caffeine
- Performing pelvic floor exercises, such as Kegels, to strengthen the pelvic muscles
- Bladder training techniques to delay urination, increase bladder capacity and improve bladder control
- Using absorbent pads or catheters to manage leaks
Pharmacological treatments:
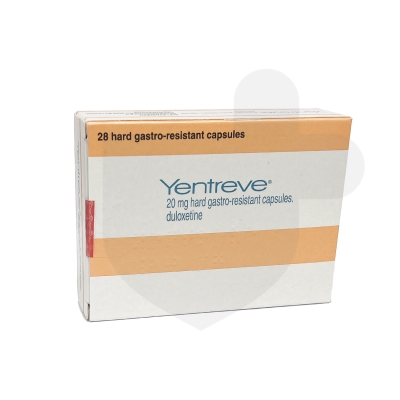
- Duloxetine, to boost muscle tone in the urethra
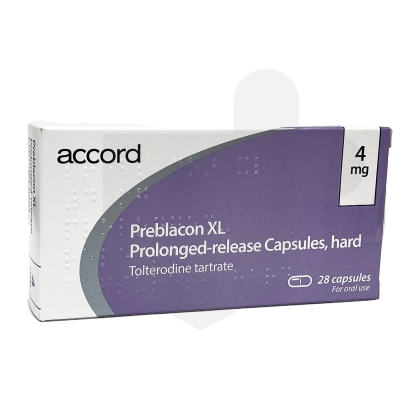
- Antimuscarinics, such as oxybutynin to control an overactive bladder
- Mirabegron, to relax bladder muscle, enhancing its ability to store urine
Be aware, the medications listed above cause side effects.
Surgical options:
- Colposuspension and sling procedures
- Urethral bulking agents
- Artificial urinary sphincter
- Botulinum toxin A injections
- Nerve stimulation therapies
Specialist services and support:
- NHS continence services
A combination of lifestyle changes, medical treatments and surgery, is often necessary, depending on the type and severity of the condition, with 80% of individuals affected by Urinary Incontinence seeing improvements with these treatments.
Living with Urinary Incontinence
Here are some practical tips for day-to-day management of Urinary Incontinence:
- Pelvic floor muscle training to strengthen the pelvic floor muscles and reduce urine leaks
- Lifestyle changes, including weight management, dietary changes, increasing fluid intake, stopping smoking and exercise modifications
- Being mindful of personal triggers
- Knowing the locations of bathrooms
- Discussing concerns with partners, family, or friends and seeking professional help if needed
- Caregivers are encouraged to seek support, including referrals to local continence services
These strategies can significantly reduce the impact of Urinary Incontinence on daily activities. For further information consult NHS Inform for comprehensive guidance.
Conclusion
Embracing strategies such as lifestyle changes, tailored therapies, and seeking professional support can lead to significant enhancements in quality of life.
Frequently asked questions about Urinary Incontinence
What can be done to treat Urinary Incontinence?
Self-help strategies and lifestyle modifications, include:
- Pelvic floor exercises
- Stopping smoking
- Exercising appropriately
- Avoiding heavy lifting
- Weight management
- Addressing constipation promptly
- Reducing caffeine and alcohol consumption
What are the different types of Urinary Incontinence?
There are 4 main types of Urinary Incontinence:
- Urgency incontinence
- Stress incontinence
- Functional incontinence
- Overflow incontinence
How can I improve my bladder control?
Performing pelvic floor muscle exercises (Kegel exercises) helps to strengthen muscles that support the bladder, helping to prevent urine leakage during activities.
Sources
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.
Related Articles
OUR CUSTOMERS VIEW
What Customers Love About Our Service
We want everyone to be happy and healthy, that’s what keeps us going. Read what some of them have to say about us.
Medicines Experts
Meet Our Medical Team
We are a broad skilled and passionate group of clinicians with experience of operating in health systems in the United Kingdom & United States. Providing excellent care and advice is at the heart of everything we do. You can read more about our medical team by visiting the medical team page or learn more about how we curate content by visiting our editorial process