Motor Neurone Disease
Get valuable insights into Motor Neurone Disease, including its causes, symptoms, prevention strategies, and treatment options, while also learning about how you can lower the cost of the medications used to treat Motor Neurone Disease.
MEDICAL INFORMATION
Motor Neurone Disease Key Facts
Motor Neurone Disease (MND), also known as Amyotrophic Lateral Sclerosis (ALS), is a progressive neurodegenerative disease that affects the nerve cells responsible for controlling voluntary muscle movement. It is a rare condition that primarily impacts the motor neurons, leading to their gradual degeneration and subsequent loss of muscle control. Here, we aim to provide you with an in-depth overview of the causes, symptoms, diagnosis, and available treatment options for Motor Neuron Disease.
What is the definition of motor neurone disease?
Motor Neurone Disease (MND) is characterized by the degeneration and eventual loss of motor neurons, which are nerve cells located in the cerebral cortex, in certain brainstem nuclei, and in the anterior horn of the spinal cord that transmit signals from the brain to the muscles, enabling voluntary movements such as walking, speaking, and swallowing. As the motor neurons deteriorate, the muscles gradually weaken, leading to difficulties with movement, coordination, and various other symptoms. Motor Neurone Disease is a rare condition with no known cure, and its progression can significantly impact a person’s quality of life.
What are the causes and risk factors associated with motor neurone disease?
Motor Neurone Disease (MND), also known as Amyotrophic Lateral Sclerosis (ALS), is a complex condition with both genetic and environmental factors contributing to its development. While the exact causes are not fully understood, researchers have identified several causes and risk factors associated with MND. These include:
Genetic Factors
Approximately 5-10% of MND cases are inherited, indicating a genetic component. Specific gene mutations have been linked to familial forms of MND, including mutations in genes such as SOD1, C9orf72, TARDBP, FUS, and others. These mutations disrupt normal cellular functions and can lead to the degeneration of motor neurons. Inherited MND tends to have an earlier age of onset and may affect multiple family members across generations. Kennedy’s disease is a genetic motor neuron disorder that primarily affects males. It belongs to a category of conditions known as lower motor neuron disorders. These disorders are characterized by disruptions in the communication between nerve cells in the brain and those in the brain stem and spinal cord
Environmental Factors
While most MND cases are not directly linked to specific environmental factors, certain exposures may increase the risk of developing the disease. These factors are thought to interact with genetic predispositions. Some environmental factors that have been studied include exposure to toxins, heavy metals (such as lead or mercury), pesticides, industrial chemicals, and other occupational exposures. However, the evidence linking specific environmental factors to MND is still evolving, and further research is needed to establish their significance
Age
Motor Neurone Disease can occur at any age, but it is more commonly diagnosed in individuals between the ages of 40 and 70. The risk of developing MND generally increases with age, with the highest incidence observed in individuals over 60
Gender
Men are slightly more likely to develop MND compared to women. However, it is important to note that the gender difference is relatively small, and MND can affect individuals of both sexes
Lifestyle Factors
Certain lifestyle factors may influence the risk of developing MND, although the evidence is not definitive. Smoking has been identified as a potential risk factor, with studies suggesting that smokers may have a higher risk of developing MND compared to non-smokers. Additionally, physical activity and maintaining a healthy weight have been associated with a reduced risk of MND, although further research is needed to fully understand these relationships
It is important to note that having one or more of these risk factors does not guarantee the development of Motor Neurone Disease. MND is a complex condition, and the interplay between genetic susceptibility, environmental factors, and other contributing factors is still being studied.
What are the different types of motor neurone disease?
The primary types of MND include:
Amyotrophic Lateral Sclerosis (ALS)
ALS is the most common form of MND. It affects both the upper motor neurons (located in the brain) and the lower motor neurons (located in the spinal cord). ALS typically presents with a combination of muscle weakness, muscle wasting, and spasticity. It can affect various regions of the body, leading to difficulties with movement, speech, swallowing, and breathing
Progressive Bulbar Palsy (PBP)
PBP primarily affects the bulbar region, which includes the muscles controlling speech, swallowing, and breathing. Individuals with PBP often experience slurred speech, difficulty swallowing, and weak facial muscles. PBP is considered a variant of ALS
Progressive Muscular Atrophy (PMA)
PMA primarily affects the lower motor neurons, resulting in muscle weakness and atrophy. Unlike ALS, PMA does not involve the upper motor neurons. PMA typically progresses more slowly, and the muscle weakness primarily affects the limbs
Primary Lateral Sclerosis (PLS)
PLS involves only the upper motor neurons, and the lower motor neurons remain unaffected. It is characterized by progressive spasticity, stiffness, and difficulties with movement and coordination. PLS progresses more slowly than ALS and primarily affects the limbs
Spinal Muscular Atrophy with Respiratory Distress (SMARD)
SMARD is a rare form of MND that affects infants. It leads to severe muscle weakness, respiratory distress, and difficulties with movement. SMARD is caused by mutations in the IGHMBP2 gene
It’s important to note that these types of MND represent different patterns of motor neuron involvement, but they share common underlying mechanisms and features of motor neuron degeneration. The symptoms and progression of MND can vary among individuals, even within the same subtype. A proper diagnosis and classification of MND are crucial for guiding treatment and management strategies.
What is the pathophysiology of motor neurone disease?
The pathophysiology of Motor Neurone Disease (MND) involves various cellular and molecular mechanisms that contribute to the degeneration of motor neurons, leading to muscle weakness and loss of voluntary muscle control. While the precise sequence of events is not fully understood, several key factors are involved in the pathogenesis of MND:
- Motor Neuron Degeneration: The hallmark of MND is the progressive degeneration of motor neurons, which are nerve cells responsible for transmitting signals from the brain to the muscles. The exact cause of motor neuron degeneration is not known, but it is believed to involve a combination of genetic, environmental, and cellular factors
- Excitotoxicity: Excitotoxicity is a process in which excessive stimulation of nerve cells by the neurotransmitter glutamate leads to their damage or death. In MND, there is an imbalance in glutamate levels or impaired clearance of glutamate from the synaptic cleft. Elevated levels of glutamate can lead to excitotoxicity, causing damage to motor neurons
- Protein Misfolding and Aggregation: Abnormal protein folding and the subsequent aggregation of specific proteins play a role in MND. Proteins such as superoxide dismutase 1 (SOD1), TAR DNA-binding protein 43 (TDP-43), and fused in sarcoma (FUS) have been implicated in MND. Mutations in these proteins or abnormal cellular handling can result in their accumulation within motor neurons, leading to toxicity and impaired cellular function
- Mitochondrial Dysfunction: Mitochondria, the energy-producing structures within cells, are essential for neuronal health and function. In MND, mitochondrial dysfunction occurs, resulting in impaired energy production, increased oxidative stress, and decreased cellular resilience. These factors contribute to motor neuron degeneration
- Neuroinflammation: Inflammatory processes within the central nervous system, particularly within motor neurons and glial cells, contribute to the progression of MND. Activated immune cells release pro-inflammatory molecules that can lead to neuroinflammation, exacerbating neuronal damage and promoting further degeneration
- Axonal Transport Deficits: Proper axonal transport, the process by which cellular materials are transported along nerve fibers, is crucial for maintaining the health and function of motor neurons. In MND, there are disruptions in axonal transport mechanisms, impairing the delivery of essential nutrients and molecules to motor neurons and contributing to their degeneration
The interplay between these mechanisms and the specific contribution of genetic and environmental factors in individual cases of MND is still an area of active research. Understanding the pathophysiology of MND is vital for developing potential therapeutic interventions to slow down or halt the progression of the disease.
What are the signs and symptoms of motor neurone disease?
Symptoms may vary among individuals, and the progression of the disease can also differ. The primary signs and early symptoms of MND include:
- Muscle Weakness: Muscle weakness is often one of the earliest and most prominent symptoms of MND. It typically begins in the limbs, affecting hands, arms, legs, or feet. As the disease progresses, the weakness spreads to other muscle groups, including those involved in speech, swallowing, and breathing
- Muscle Wasting: Over time, the muscles affected by MND may start to waste away (atrophy) due to the loss of motor neurons. This leads to a visible reduction in muscle size and strength
- Spasticity: Many individuals with MND experience muscle stiffness and spasticity. This can result in muscle cramps, involuntary muscle twitches (fasciculations), and difficulty with movement and coordination
- Fatigue and Weakness: Fatigue and general weakness are common in MND. It may feel difficult to carry out daily activities that were once effortless
- Difficulties with Speech and Swallowing: MND can affect the muscles involved in speech and swallowing. Speech may become slurred or difficult to understand (dysarthria), and individuals may experience trouble swallowing (dysphagia). This can lead to choking or aspiration
- Breathing Difficulties: As the disease progresses, the muscles responsible for breathing can weaken, leading to breathing difficulties. Shortness of breath, respiratory problems, and the need for breathing support may arise
- Changes in Reflexes: MND can cause changes in reflexes. The affected reflexes may become exaggerated (hyperreflexia) or diminished
- Loss of Motor Control: As the disease advances, individuals may experience a loss of fine motor control, leading to difficulties with tasks that require precise movements, such as buttoning a shirt or writing
It’s important to note that the presentation and progression of symptoms can vary among individuals. MND is a progressive disease, and symptoms worsen over time. Early recognition of these signs and symptoms is crucial for early diagnosis and appropriate management. If any of these symptoms are present, it is advisable to seek medical attention for a thorough evaluation.
What are the stages of motor neurone disease (UK)?
In the UK, the stages of Motor Neurone Disease (MND) are commonly categorized into three main stages: early, middle, and late. These stages help provide a general framework to understand the progression of the disease. It’s important to note that the progression and specific symptoms can vary among individuals, and not everyone will experience MND in the same way. The stages are as follows:
Early Stage
- Individuals in the early stage of MND typically experience mild symptoms, which may include muscle weakness, fatigue, and subtle changes in motor function
- Symptoms may initially affect one specific region, such as the hands, arms, or legs, before spreading to other areas over time
- Some individuals may experience speech and swallowing difficulties, including slurred speech and problems with eating and drinking
- Despite the presence of symptoms, individuals in the early stage can often maintain a level of independence and continue with their daily activities
Middle Stage
- The middle stage of MND is characterized by an increase in the severity and progression of symptoms
- Muscle weakness and wasting become more pronounced, leading to greater difficulties with movement, coordination, and mobility
- Speech and swallowing difficulties may worsen, requiring additional support or alternative communication methods
- Breathing function can be affected, and individuals may require respiratory support, such as non-invasive ventilation (NIV), to assist with breathing
- The middle stage often necessitates greater reliance on assistive devices, such as mobility aids and communication devices, to maintain independence and quality of life
Late Stage
- In the late stage of MND, symptoms become significantly more severe, and individuals may experience profound physical limitations
- Muscle weakness and wasting are extensive, leading to severe difficulties with mobility and the ability to perform daily activities independently
- Speech may become extremely challenging or impossible, and alternative communication methods, such as eye-tracking devices or communication boards, may be required
- Swallowing difficulties may worsen, necessitating a feeding tube for nutrition and hydration
- Breathing function is severely compromised, and individuals may require invasive ventilation through a tracheostomy to support respiration
- In the late stage, individuals typically require extensive care and support, often with the assistance of healthcare professionals and caregivers
What are the stages of motor neurone disease (US)?
In the United States, Motor Neurone Disease (MND), also known as Amyotrophic Lateral Sclerosis (ALS), is commonly categorized into four stages based on the functional abilities and progression of symptoms. These stages provide a general framework to understand the typical course of the disease. However, it’s important to note that the progression and specific symptoms can vary among individuals. The stages are as follows:
Stage 1 – Early Stage
- In the early stage, individuals experience minimal symptoms, which may include muscle weakness, fatigue, or subtle changes in motor function
- Symptoms may initially affect one specific region, such as the hands, arms, or legs, before spreading to other areas over time
- Individuals in this stage can typically perform daily activities independently with minor difficulties
- Speech and swallowing abilities are usually normal.
Stage 2 – Mild Stage
- In the mild stage, symptoms become more noticeable, and there is an increase in muscle weakness and motor impairment
- Individuals may experience difficulties with walking, climbing stairs, or performing fine motor tasks
- Speech may become mildly affected, with slight changes in clarity or voice projection
- Swallowing abilities may be slightly impaired, leading to occasional swallowing difficulties with certain textures or consistencies of food and drink
- Despite these challenges, individuals can still perform most activities of daily living with some assistance or modifications
Stage 3 – Moderate Stage
- The moderate stage is characterized by a significant increase in functional limitations and mobility difficulties
- Muscle weakness and wasting become more pronounced, affecting multiple regions of the body
- Individuals may require assistive devices such as wheelchairs, walkers, or braces to aid with mobility
- Speech may be noticeably affected, with increased difficulty articulating words and reduced voice volume
- Swallowing difficulties become more prominent, necessitating dietary modifications and potentially requiring the use of a feeding tube
- Breathing function remains relatively unaffected in this stage
Stage 4 – Severe Stage
- The severe stage represents the most advanced stage of MND, with significant functional limitations and profound physical impairments
- Muscle weakness and wasting are extensive, leading to severe difficulties with mobility and limited ability to perform activities of daily living independently
- Individuals may be completely reliant on assistive devices and require 24/7 caregiving support
- Speech becomes severely impaired or lost entirely, requiring alternative communication methods
- Swallowing difficulties are significant, and individuals often require a feeding tube for nutrition and hydration
- Breathing function is severely compromised, and individuals may require invasive ventilation through a tracheostomy to support respiration
How is motor neurone disease diagnosed?
Following diagnosis, the life expectancy for individuals with MND typically ranges between one to five years, although 10% of those diagnosed can live for 10 years or more. The diagnosis of Motor Neurone Disease (MND) involves a comprehensive evaluation that includes medical history, physical examination, and various tests to assess motor function, rule out other conditions, and support the diagnosis. The diagnostic process typically involves the following:
- Medical History: The healthcare provider or Neurology specialist will review the individual’s medical history, including the onset and progression of symptoms, family history of MND or related conditions, and any potential risk factors or exposures
- Physical Examination: A thorough physical examination is conducted to assess motor function, muscle strength, reflexes, coordination, and other neurological functions. The healthcare provider will observe and assess any muscle weakness, muscle wasting, spasticity, or changes in reflexes
- Electromyography (EMG): EMG is a test that measures the electrical activity of muscles and can help detect abnormalities in the functioning of motor neurons. It involves inserting fine needle electrodes into specific muscles to evaluate their electrical signals. Abnormal EMG findings, such as signs of denervation or reinnervation, can support the diagnosis of MND
- Nerve Conduction Study (NCS): NCS is often performed alongside EMG and evaluates the speed and strength of the electrical signals traveling through the nerves. It helps assess the integrity and function of the peripheral nerves and can aid in the diagnosis by ruling out other nerve-related conditions
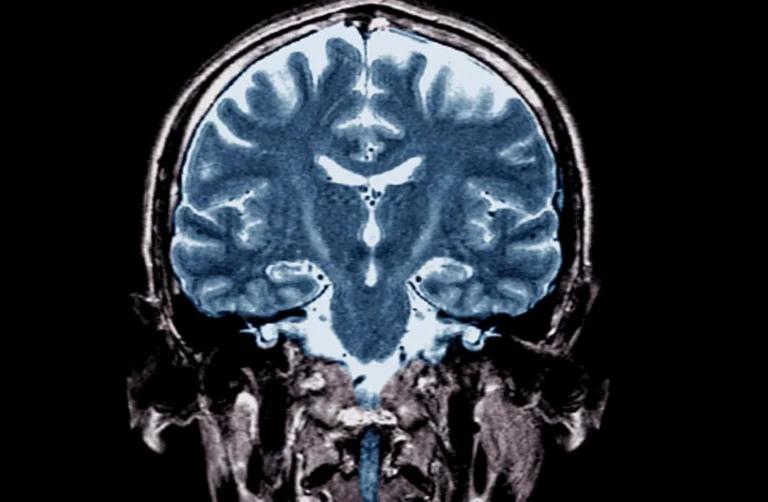
- Imaging Studies: Imaging techniques like Magnetic Resonance Imaging (MRI) or computed tomography (CT) scans may be performed to rule out other conditions that can mimic MND, such as spinal cord compression or tumors. These imaging studies are not diagnostic for MND but help exclude other potential causes of symptoms
- Laboratory Tests: Blood tests and urine tests may be ordered to rule out other possible causes of symptoms, such as thyroid disorders, kidney disease, vitamin deficiencies, or autoimmune conditions
- Clinical Criteria: The diagnosis of MND is primarily based on clinical criteria and the presence of progressive, widespread signs of upper and lower motor neuron dysfunction. The revised El Escorial criteria and the Awaji-Shima criteria are commonly used to classify and support the diagnosis of MND
It is important to note that MND is a complex condition, and the diagnosis can be challenging due to the similarity of symptoms with other neurological disorders. The diagnostic process often involves the collaboration of neurologists, specialists in neuromuscular disorders, and other healthcare professionals with expertise in MND. Early diagnosis and appropriate management are crucial for optimizing care and support for individuals with MND.
How is motor neurone disease prevented?
Currently, there is no known way to prevent Motor Neurone Disease (MND) as the exact causes of the disease are not fully understood. However, there are some general recommendations that may promote overall health and well-being, which could potentially have indirect effects on reducing the risk or delaying the onset of MND. These recommendations include:
- Healthy Lifestyle: Maintaining a healthy lifestyle is important for overall well-being. This includes eating a balanced diet, engaging in regular physical activity, and avoiding excessive alcohol consumption and smoking
- Environmental Exposures: While the specific environmental factors associated with MND are not fully identified, minimizing exposure to potential toxins, chemicals, and pollutants in the environment may be beneficial. This can involve practicing proper safety measures in the workplace and avoiding exposure to harmful substances
- Genetic Counseling: In cases where there is a known family history of MND or identified genetic mutations associated with the disease, genetic counseling can provide individuals and families with information about the risks and potential preventive measures. Genetic counseling can help individuals make informed decisions regarding family planning and understand the implications of inherited genetic factors
- Research and Clinical Trials: Continued research into the causes, risk factors, and potential preventive strategies for MND is essential. Participation in clinical trials and studies aimed at understanding MND can contribute to advancing knowledge in the field and potentially identifying preventive measures in the future
It is important to note that while adopting a healthy lifestyle and taking preventive measures may promote overall health, they cannot guarantee the prevention of MND. Given the complex nature of the disease, it is advisable to focus on raising awareness, supporting research efforts, and providing appropriate care and support for individuals and families affected by MND.
What are the treatment and management options for motor neurone disease?
While there is currently no cure for Motor Neurone Disease (MND), there are treatment and management options available to help alleviate symptoms, improve quality of life, and provide supportive care. The treatment and management options for MND include:
Medications
- Riluzole: This is the only medication approved by the FDA for the treatment of MND. It works by reducing the release of glutamate, a neurotransmitter associated with nerve cell damage Riluzole has been shown to modestly slow the progression of the disease and extend survival in some individuals
- Edaravone: Another FDA-approved medication, Edaravone, is an intravenous infusion administered over a series of treatment cycles. It is an antioxidant that can help reduce oxidative stress and slow the decline in function. It has shown potential in slowing functional decline in individuals with MND
Physical and Occupational Therapy
- Physical Therapy: Physical therapy focuses on maintaining and improving mobility, range of motion, and strength through targeted exercises, stretching, and assistive devices. It aims to optimize functional abilities and reduce the risk of complications such as joint contractures and muscle atrophy
- Occupational Therapy: Occupational therapy addresses the practical aspects of daily living, including activities such as dressing, bathing, and using assistive devices. Occupational therapists can provide strategies, adaptations, and assistive technology to help individuals maintain independence and enhance their quality of life
Speech and Swallowing Therapy
- Speech Therapy: Speech and language therapists work with individuals with MND to address difficulties with speech clarity, voice projection, and communication. They may provide techniques, exercises, and assistive communication devices to improve speech intelligibility and alternative communication methods as needed
- Swallowing Therapy: Swallowing therapists (also known as dysphagia therapists) help individuals manage swallowing difficulties and prevent complications such as choking or aspiration. They can provide exercises, modifications in diet consistency, and guidance on safe swallowing techniques
Assistive Devices and Adaptive Equipment
- Mobility Aids: Depending on the level of mobility impairment, individuals may benefit from mobility aids such as wheelchairs, walkers, scooters, or orthotic devices to assist with movement and maintain independence
- Communication Aids: As speech becomes challenging, augmentative and alternative communication (AAC) devices, eye-tracking systems, or communication boards can help individuals communicate effectively
- Assistive Technology: Various assistive technology devices, including computer access devices, environmental control systems, and home modifications, can enhance independence and improve the ability to perform daily activities
Respiratory Support
- Non-Invasive Ventilation (NIV): As respiratory muscles weaken, NIV, delivered through a mask, can provide breathing support during sleep and rest, improving oxygenation and reducing respiratory distress
- Invasive Ventilation: In advanced stages of MND, when breathing becomes severely compromised, individuals may opt for invasive ventilation through a tracheostomy. This involves the insertion of a breathing tube directly into the windpipe
Palliative Care and Supportive Measures
- Palliative care focuses on managing symptoms, providing emotional support, addressing psychosocial needs, and enhancing quality of life for individuals and their families throughout the course of the disease
- Supportive measures, including psychological counseling, support groups, and access to community resources, can play a vital role in addressing the emotional, social, and practical aspects of living with MND
What are the complications of motor neurone disease?
Motor Neurone Disease (MND) can give rise to various complications as the disease progresses. These complications can significantly impact an individual’s quality of life and require appropriate management and support. Some common complications associated with MND include:
- Respiratory Complications: As MND affects the muscles involved in breathing, respiratory complications can arise. Weakness in the diaphragm and other respiratory muscles can lead to reduced lung capacity and compromised breathing. This can result in shortness of breath, respiratory distress, and an increased risk of respiratory infections
- Swallowing Difficulties (Dysphagia): MND can cause weakness in the muscles responsible for swallowing (bulbar muscles). Dysphagia, or difficulty swallowing, can lead to problems with eating and drinking. It can increase the risk of choking, aspiration (inhaling food or liquids into the lungs), and malnutrition
- Communication Challenges: As MND progresses, individuals may experience difficulties with speech due to muscle weakness and impaired control of the vocal cords and facial muscles. Speech may become slurred or difficult to understand (dysarthria), leading to communication challenges. Alternative communication methods or assistive devices may be required
- Nutritional Complications: Dysphagia and difficulties with chewing and swallowing can result in inadequate nutrition and hydration. Malnutrition and dehydration can lead to weight loss, weakness, fatigue, and a compromised immune system
- Mobility Limitations: Progressive muscle weakness and loss of motor control can impair mobility and make walking and other movements challenging. This can lead to a higher risk of falls, injuries, and difficulties with activities of daily living
- Contractures and Joint Stiffness: Immobility and muscle weakness can contribute to the development of joint contractures (shortening and tightening of muscles and tendons) and joint stiffness. These can result in reduced range of motion, pain, and difficulties with positioning and mobility
- Emotional and Psychological Impact: The physical and functional limitations of MND, along with the knowledge of the disease’s progressive nature, can have a significant emotional and psychological impact on individuals and their families. Feelings of sadness, anxiety, depression, frustration, and grief are common and may require psychological support and counseling
- Reduced Quality of Life: The cumulative impact of the complications associated with MND can lead to a reduced quality of life. Challenges with mobility, communication, breathing, eating, and daily activities can significantly affect independence, social interactions, and overall well-being
What medications are used in motor neurone disease?
- Riluzole (Rilutek): Riluzole is the only FDA-approved medication for ALS. It may help slow down the progression of the disease by reducing glutamate levels in the brain
- Edaravone (Radicava): Edaravone is another FDA-approved medication for ALS. It is administered intravenously and is thought to have antioxidant and neuroprotective properties
- Muscle relaxants: Medications such as baclofen, tizanidine, or diazepam may be prescribed to manage muscle stiffness, cramps, or spasticity that can occur in ALS
- Saliva-thinning medications: Medications like glycopyrrolate may be prescribed to reduce excessive saliva production and drooling
- Medications for respiratory symptoms: Medications such as bronchodilators, mucolytics, or antibiotics may be prescribed to manage respiratory symptoms and prevent respiratory infections
Promising research and future direction of motor neurone disease
Promising research and future directions in Motor Neurone Disease (MND) focus on understanding the underlying mechanisms of the disease, developing new treatment approaches, and improving patient care. Here are some areas of research and potential advancements in MND:
- Genetic Studies: Researchers are continuing to investigate the genetic factors involved in MND. The discovery of new genes and genetic mutations associated with the disease provides opportunities for better understanding its pathogenesis and developing targeted therapies
- Stem Cell Research: Stem cell therapy holds promise in MND research. Scientists are exploring the use of different types of stem cells, such as induced pluripotent stem cells (iPSCs) or neural stem cells, to replace damaged motor neurons or provide neuroprotective effects. This avenue of research aims to restore motor function and slow down disease progression
- Gene Therapy: Gene therapy involves delivering functional genes or gene-modifying agents to target and correct the genetic mutations associated with MND. This approach aims to halt or slow the progression of the disease by addressing the underlying genetic causes
- Neuroprotective Strategies: Researchers are investigating various neuroprotective strategies to prevent or delay motor neuron degeneration in MND. These approaches involve the use of drugs, growth factors, antioxidants, and other agents that can protect motor neurons from damage and enhance their survival
- Biomarkers and Early Detection: The identification of reliable biomarkers for MND could aid in early diagnosis, tracking disease progression, and evaluating treatment responses Researchers are exploring different biomarkers, including genetic markers, imaging techniques, blood-based markers, and cerebrospinal fluid biomarkers, to improve diagnostic accuracy and enable earlier intervention
- Therapeutic Targets: Ongoing research aims to identify novel therapeutic targets within the cells and molecular pathways involved in MND. By better understanding the mechanisms of motor neuron degeneration, researchers can develop targeted therapies that interfere with disease progression and improve outcomes
It’s important to note that research in MND is a rapidly evolving field, and advancements are continually being made. While there is currently no cure for MND, these research efforts offer hope for developing more effective treatments, interventions, and ultimately finding a cure for this devastating disease.
What motor neurone disease support organisations are there available to support me in the UK?
- Motor Neurone Disease Association (MNDA): The MNDA is the largest charity organization in the UK dedicated to supporting individuals with MND. They provide a range of services, including support for individuals and families, information resources, access to equipment and grants, advocacy, and research funding. They also offer a helpline and local support groups
- MND Scotland: MND Scotland is a charity organization that provides support and information for individuals with MND in Scotland. They offer practical advice, emotional support, advocacy, and funding for research. They also provide specialized services, such as MND Specialist Nurses and financial support grants
- MND Association of Wales: The MND Association of Wales is a charity organization that provides support and resources for individuals with MND in Wales. They offer information, advocacy, equipment loans, and financial assistance. They also organize events and activities to raise awareness and funds for MND research
- MND Northern Ireland: MND Northern Ireland is a charity organization that supports individuals with MND in Northern Ireland. They provide information resources, advocacy, equipment loans, and financial assistance. They also organize events and campaigns to raise awareness and improve services for people with MND
- My Name’5 Doddie Foundation: The My Name’5 Doddie Foundation is a charity established by former Scottish rugby player Doddie Weir, who has MND. The foundation focuses on raising funds for MND research, improving awareness, and supporting individuals and families affected by MND
What motor neurone disease support organisations are there available to support me in the US?
- The ALS Association: The ALS (amyotrophic lateral sclerosis) Association is the largest nonprofit organization in the US dedicated to fighting ALS. They provide comprehensive support and services to individuals with ALS and their families, including support groups, equipment loan programs, financial assistance, care services, and research funding
- MDA – Muscular Dystrophy Association: The Muscular Dystrophy Association supports individuals and families affected by a range of neuromuscular diseases, including ALS. They provide resources, support groups, and assistance with medical equipment, clinic visits, and research funding
- ALS Therapy Development Institute (ALS TDI): ALS TDI is a nonprofit biotech organization focused on discovering and developing treatments for ALS. They provide resources, educational materials, clinical trial information, and support services for individuals with ALS
- Team Gleason: Team Gleason is a nonprofit organization founded by former NFL player Steve Gleason, who has ALS. They offer a range of support programs, including providing access to assistive technology, creating awareness about ALS, and funding research
- Les Turner ALS Foundation: The Les Turner ALS Foundation is a nonprofit organization based in the Chicago area. They provide support and resources for individuals with ALS and their families, including equipment loans, support groups, counseling services, and education programs
- Project ALS: Project ALS is a nonprofit research organization dedicated to finding a cure for ALS. They fund research initiatives, provide patient and family support, and collaborate with scientists and clinicians to advance understanding and treatment options for ALS
Summary
Motor Neuron Disease is a progressive neurodegenerative disorder that affects motor neurons, leading to muscle weakness, wasting, and loss of control. While the causes are not fully understood, genetic and environmental factors likely contribute to its development. Early diagnosis and a multidisciplinary approach involving medications, therapy, and supportive care can help manage symptoms and enhance the quality of life for individuals with Motor Neuron Disease. Ongoing research offers hope for future advancements in treatment and potential cures for this debilitating condition.
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.