Motor neurone disease (MND) is a rare and devastating neurological condition that affects the nerve cells responsible for controlling our voluntary muscle movements. As this progressive disorder gradually weakens and destroys these motor neurons, it can lead to a gradual decline in an individual’s ability to walk, talk, swallow, and even breathe. While MND may not be common, it’s crucial to be aware of the potential early warning signs, as prompt medical attention can make a significant difference in managing the condition and improving quality of life.
Understanding the motor system and motor neurones
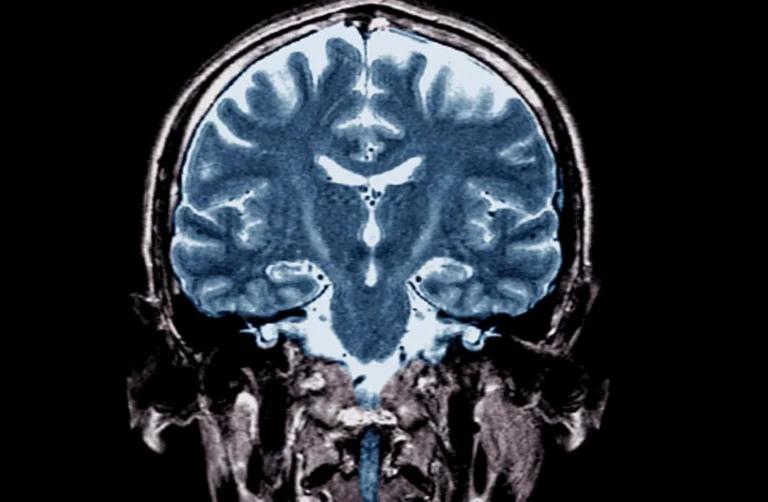
The motor system is a complex network of nerve cells and pathways that work together to control our voluntary movements. At the core of this system are the motor neurones, which are divided into two main categories: upper motor neurones located in the brain, and lower motor neurones situated in the brainstem and spinal cord. These specialised cells transmit signals from the central nervous system to the muscles, enabling us to perform a wide range of physical actions.
In MND, the degeneration and loss of function in these motor neurones disrupt the communication between the brain, spinal cord, and muscles, leading to the characteristic symptoms of the disease. As the condition progresses, the affected individual may experience increasing difficulty with various everyday tasks, such as gripping objects, maintaining balance, and even speaking or swallowing.
Early symptoms of motor neurone disease
The early stages of MND can often be subtle and easily mistaken for other, more common health issues. However, recognising these early warning signs is crucial for seeking prompt medical attention and obtaining an accurate diagnosis. Some of the most common early symptoms of MND include:
Muscle twitching and fasciculations
The noticeable first symptom of MND is the presence of involuntary muscle twitches, known as fasciculations. These small, visible contractions of the muscle fibres can occur in various parts of the body, such as the hands, arms, legs, or even the tongue. While fasciculations can also be associated with other conditions, such as fatigue or stress, their persistence and spread to different muscle groups may be an early indicator of MND.
Muscle weakness and wasting
As the motor neurones deteriorate, the muscles they control begin to weaken and waste away. This can manifest in a variety of ways, such as difficulty gripping objects, tripping or stumbling more frequently, or a noticeable reduction in the size of the affected muscles. These changes are often first observed in the hands, feet, or limbs, and may gradually spread to other parts of the body as the condition progresses.
Speech and swallowing difficulties
The muscles involved in speech, swallowing, and coughing can also be affected by MND. Individuals may experience slurred or faint speech, difficulty swallowing food or liquids, and an increased risk of choking or aspiration (inhaling food or saliva into the lungs). These symptoms can have a significant impact on an individual’s daily life and overall health, as they can lead to malnutrition, dehydration, and respiratory complications.
Emotional and cognitive changes
While MND primarily affects the motor system, some individuals may also experience changes in their emotional and cognitive functioning. This can include uncontrollable laughing or crying, known as emotional lability, as well as mild difficulties with memory, decision-making, or problem-solving. These cognitive and behavioural changes are more common in certain types of MND, such as frontotemporal dementia, and may become more pronounced as the disease progresses.
Breathing difficulties
In the later stages of MND, the weakening of the muscles responsible for breathing can lead to respiratory problems, such as shortness of breath, frequent chest infections, and difficulty sleeping. This can result in a range of secondary symptoms, including morning headaches, poor concentration, and fatigue, which can further impact an individual’s quality of life.
Diagnosing motor neurone disease
Diagnosing MND can be a complex and challenging process, as there is no single test that can definitively confirm the condition. Instead, healthcare professionals typically rely on a combination of medical history, physical examination, and various diagnostic tests to rule out other potential causes and arrive at an accurate diagnosis.
Medical history and physical examination
The initial step in the diagnostic process is a thorough review of the individual’s medical history and a comprehensive physical examination. The healthcare provider will ask about the onset and progression of symptoms, any family history of neurological conditions, and any other underlying health issues. They will also perform a detailed neurological assessment to evaluate muscle strength, reflexes, and coordination.
Diagnostic tests
If MND is suspected based on the initial evaluation, the healthcare provider may order a series of diagnostic tests to help confirm the diagnosis and rule out other conditions. These tests may include:
- Electromyography (EMG) and Nerve Conduction Studies: These tests measure the electrical activity in the muscles and nerves, providing information about the health and function of the motor neurones
- Magnetic Resonance Imaging (MRI): MRI scans of the brain and spinal cord can help identify any structural abnormalities or rule out other neurological conditions
- Blood and Genetic Tests: Blood tests can be used to check for certain biomarkers or genetic mutations associated with MND, while genetic testing can help identify inherited forms of the disease
- Lumbar Puncture (Spinal Tap): In some cases, a sample of the cerebrospinal fluid may be collected and analysed to aid in the diagnostic process
Types of MND
While MND is a broad term that encompasses several related conditions, there are distinct types that differ in their specific symptoms, progression, and underlying causes. Understanding these different forms of MND can help individuals and their healthcare providers develop a more tailored approach to managing the disease.
Amyotrophic Lateral Sclerosis (ALS)
Also known as Lou Gehrig’s disease, ALS is the most common and severe form of MND. It affects both the upper and lower motor neurones, leading to a rapid and progressive loss of muscle control and function.
Progressive Muscular Atrophy (PMA)
PMA is a less common subtype of MND that primarily affects the lower motor neurones, resulting in slower disease progression and a focus on muscle wasting and weakness.
Progressive Bulbar Palsy (PBP)
PBP is characterised by the degeneration of motor neurons in the brainstem, which can lead to difficulties with speech, swallowing, and emotional control.
Primary Lateral Sclerosis (PLS)
PLS is a rare form of MND that specifically targets the upper motor neurones, causing muscle stiffness, spasticity, and slowness of movement, but without the characteristic muscle wasting.
Spinal Muscular Atrophy (SMA)
SMA is a genetic form of MND that primarily affects the lower motor neurones, leading to progressive muscle weakness and atrophy, often with onset in childhood or adolescence.
Understanding the distinct features of these MND subtypes can help healthcare providers tailor the diagnostic process, develop appropriate treatment strategies, and provide more accurate prognosis and support for individuals affected by the condition.
Treatment of MND
Unfortunately, there is no cure for MND, and the available treatments are primarily focused on managing the symptoms and improving the individual’s quality of life. However, an approach involving various healthcare professionals can make a significant difference in the care and support provided to individuals with MND.
Medications
The only medication specifically approved for the treatment of MND is riluzole, which has been shown to slightly slow the progression of the disease and modestly increase life expectancy. Additionally, healthcare providers may prescribe other medications to help manage symptoms such as muscle spasms, excessive saliva production, and emotional lability.
Supportive therapies
A range of supportive therapies can be beneficial for individuals with MND, including:
- Physical and occupational therapy to maintain muscle strength, improve mobility, and adapt to changing physical needs
- Speech and language therapy to address communication and swallowing difficulties
- Respiratory therapy and assistive devices to support breathing and prevent respiratory complications
- Nutritional counselling and support to maintain a healthy diet and prevent weight loss
- Emotional and psychological support to help individuals and their families cope with the challenges of the disease
Assistive technology
As MND progresses, individuals may require the use of various assistive devices and technologies to maintain their independence and quality of life. These can include mobility aids, communication devices, and adaptive equipment for daily living activities.
Palliative care
In the later stages of MND, palliative care and hospice services can provide essential support, pain management, and comfort for individuals and their families. This holistic approach aims to improve the quality of life and ensure that the individual’s wishes and preferences are respected during the final stages of the disease.
Early Intervention and ongoing support
Early recognition of the symptoms of MND and prompt medical attention are crucial for managing the condition effectively. By seeking timely diagnosis and accessing appropriate support, individuals with MND can potentially slow the disease’s progression, maintain their independence for longer, and improve their overall quality of life.
Moreover, the involvement of a multidisciplinary team of healthcare professionals, including neurologists, physical and occupational therapists, speech and language therapists, and palliative care specialists, can provide a comprehensive and personalised approach to managing the various aspects of MND.
Ongoing support and education for individuals with MND and their caregivers are also vital. Organisations such as the Motor Neurone Disease Association (MNDA) and the ALS Association offer a wealth of resources, including information on the latest research, access to support groups, and guidance on navigating the practical and emotional challenges of living with this condition.
Conclusion
Motor neurone disease is a rare and devastating condition that can have a profound impact on an individual’s physical, emotional, and cognitive well-being. However, by being aware of the early warning signs, seeking prompt medical attention, and accessing a range of supportive therapies and resources, individuals with MND can work to manage the disease and maintain the best possible quality of life.
Sources
- Early signs of MND – MND Association
- Motor neurone disease – NHS
- Motor Neurone Disease (MND) – Fact Sheet | Health Information – Brain & Spine Foundation
- Motor Neuron Diseases – National Institute of Neurological Disorders and Stroke
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.