Motor neurone diseases (MNDs) are a diverse group of progressive neurological disorders characterised by the gradual degeneration and eventual death of motor neurons, the specialised nerve cells responsible for controlling voluntary muscle movements. These debilitating conditions can deeply impact daily life, including walking, speaking, swallowing, and even breathing. Among the spectrum of MNDs, amyotrophic lateral sclerosis (ALS), commonly known as Lou Gehrig’s disease, stands out as a particularly devastating form, affecting both upper and lower motor neurons.
Understanding motor neurons
These specialised nerve cells serve as the vital link between the brain and the muscles, facilitating voluntary movements through a complex network of communication pathways.
Motor neurons can be broadly categorised into two distinct groups:
- Upper Motor Neurons (UMNs): These neurons originate in the brain’s movement areas and extend their projections to the brainstem or spinal cord, acting as the command centre for voluntary muscle movements
- Lower Motor Neurons (LMNs): These neurons extend from the brainstem or spinal cord directly to the muscles throughout the body, transmitting the signals received from the UMNs and triggering muscle contractions
The proper functioning of both UMNs and LMNs is crucial for seamless voluntary muscle control and coordination.
Classifying Motor Neuron Diseases
MNDs are classified based on the specific motor neuron affected, which can involve either UMNs, LMNs, or a combination of both.
Disorders affecting lower motor neurons
When LMNs are primarily affected, the muscles they stimulate begin to weaken and shrink in size. This can show up as muscle twitching, known as fasciculations, and progressive loss of muscle strength and control. Examples of MNDs primarily affecting LMNs include:
- Progressive Muscular Atrophy (PMA): A rare subtype of ALS characterised by gradual damage to the LMNs, leading to muscle weakness and wasting
- Spinal Muscular Atrophy (SMA): A group of inherited disorders caused by mutations in the survival motor neuron gene (SMN1), resulting in the deterioration of LMNs and followed by muscle weakness and atrophy
- Kennedy’s Disease: An inherited LMN disorder affecting primarily men, caused by mutations in the androgen (male sex hormone) receptor gene
Disorders affecting upper motor neurons
When UMNs are selectively affected, individuals may experience muscle stiffness (spasticity), overactive reflexes, and difficulties with coordinated movements, despite the absence of significant muscle atrophy. Examples of MNDs primarily affecting UMNs include:
- Primary Lateral Sclerosis (PLS): A rare disorder characterised by the degeneration of UMNs, leading to progressive muscle stiffness, weakness, and impaired coordination
- Hereditary Spastic Paraplegia (HSP): A group of inherited disorders characterised by spasticity and weakness predominantly in the legs, resulting in progressive difficulty walking
Disorders affecting both upper and lower motor neurons
In some MNDs, both UMNs and LMNs are affected, leading to a combination of symptoms, including muscle weakness, atrophy, spasticity, and impaired coordination. The most well-known disorder in this category is:
- Amyotrophic Lateral Sclerosis (ALS): A rapidly progressive disorder affecting both UMNs and LMNs, leading to progressive muscle weakness, paralysis, and eventually respiratory failure
Amyotrophic Lateral Sclerosis (ALS)
Amyotrophic lateral sclerosis (ALS), often referred to as Lou Gehrig’s disease, is a devastating form of MND that affects both UMNs and LMNs. It is characterised by a relentless progression of muscle weakness, paralysis, and eventual respiratory failure.
Risk factors
ALS is considered a rare disease, with an estimated incidence of 2 per 100,000 individuals per year and a prevalence of approximately 6 per 100,000 individuals. While the exact causes of ALS are not fully understood, several risk factors have been identified:
- Genetics: Approximately 10% of ALS cases are familial, meaning they are inherited through genetic mutations passed down from a family member. The most common gene mutations associated with familial ALS are found in the C9ORF72 and SOD1 genes
- Age: The risk of developing ALS increases with age, with the average onset occurring around 55 years old
- Sex: Before the age of 65, ALS is slightly more common in men than women, but this difference disappears after age 70
- Environmental factors: Potential environmental risk factors, such as smoking, exposure to certain toxins or chemicals, and military service, have been associated with an increased risk of developing ALS, although further research is needed to establish definitive links
Symptoms
The symptoms of ALS can vary among individuals, but they typically involve progressive muscle weakness, atrophy, and spasticity. Common initial symptoms may include:
- Difficulty walking or performing daily activities
- Tripping or falling frequently
- Weakness in the arms, hands, or legs
- Slurred speech or trouble swallowing
- Muscle cramps and twitching (fasciculations)
As the disease progresses, individuals with ALS may experience:
- Rapid loss of muscle control and paralysis
- Breathing difficulties due to respiratory muscle weakness
- Cognitive and behavioural changes (in some cases, frontotemporal dementia)
The average survival time from symptom onset is typically 3 years, although some individuals may live 5 years or longer with the disease. Unfortunately, there is currently no cure for ALS, and treatment focuses on managing symptoms and maintaining quality of life through multidisciplinary care.
Genetics and familial ALS
While the majority of ALS cases are considered sporadic, meaning they occur without a known family history, approximately 10% of cases are classified as familial ALS. Specific gene mutations have been identified as the underlying cause in these cases.
Familial ALS is typically inherited in an autosomal dominant pattern, which means that each child or sibling of an affected individual has a 50% chance of inheriting the genetic mutation and potentially developing the disease.
The most commonly identified gene mutations associated with familial ALS include:
- C9ORF72: This gene mutation accounts for a significant proportion of familial ALS cases and is also found in some cases of sporadic ALS
- SOD1 (Superoxide Dismutase 1): Mutations in this gene were among the first identified genetic causes of ALS
It is important to note that genetic testing and counselling are recommended for individuals with a family history of ALS or those diagnosed with sporadic ALS who carry known ALS-associated gene mutations. This information can help assess the risk for family members and guide reproductive decisions.
Diagnosis
Diagnosing MNDs can be challenging, as symptoms may initially resemble those of other neurological or muscular disorders. However, a combination of clinical evaluations, diagnostic tests, and careful monitoring of symptom progression can aid in accurate diagnosis.
Diagnostic Procedures
The diagnostic process for MNDs typically involves the following steps:
- Medical history and physical examination: A detailed medical history and thorough neurological examination are essential to assess motor function, muscle strength, reflexes, and coordination
- Electromyography (EMG) and nerve conduction studies: These tests evaluate the electrical activity of muscles and nerves, helping to distinguish between nerve and muscle disorders
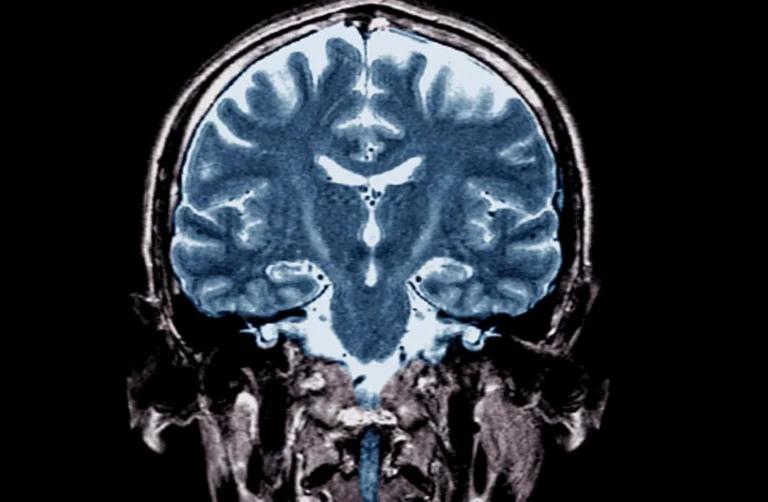
- Imaging tests: Magnetic resonance imaging (MRI) and other imaging techniques may be used to rule out other conditions with similar symptoms, such as brain or spinal cord tumours, inflammation, or vascular abnormalities
- Laboratory tests: Blood, urine, or cerebrospinal fluid tests can help exclude other potential causes of symptoms
- Genetic testing: In cases where a genetic component is suspected, genetic testing may be performed to identify specific gene mutations associated with MNDs
Treatment
While there is currently no cure for most MNDs, various treatment approaches aim to manage symptoms, maintain quality of life, and slow disease progression when possible.
- Medications: Several medications have been approved to target specific aspects of MNDs, such as slowing disease progression in ALS or addressing gene mutations in SMA and genetic forms of ALS
- Supportive therapies: Physical and occupational therapy, speech therapy, and assistive devices (e.g., mobility aids, communication devices, and feeding tubes) can help individuals adapt to the changing needs and maintain independence for as long as possible
- Symptom management: Medications and interventions may be used to alleviate muscle spasticity, excessive saliva production, breathing difficulties, and other symptoms associated with MNDs
- Multidisciplinary care: A team-based approach involving neurologists, physical therapists, occupational therapists, respiratory therapists, speech therapists, and social workers is crucial for comprehensive care and support throughout the disease course
Ongoing research
Extensive research efforts are underway to unravel the underlying mechanisms of MNDs, identify potential biomarkers, and develop effective treatments and interventions. Some areas of active investigation include:
- Genetic studies: Researchers are working to identify additional gene mutations and understand how they contribute to the development and progression of MNDs, paving the way for targeted therapies
- Biomarker discovery: The identification of reliable biomarkers (biological indicators of disease) can aid in early diagnosis, monitoring disease progression, and evaluating the effectiveness of potential treatments
- Novel therapeutic approaches: Various therapeutic strategies are being explored, including gene therapy, stem cell therapy, and the development of neuroprotective agents to slow or halt the degeneration of motor neurons
- Clinical trials: Numerous clinical trials are underway to evaluate the safety and efficacy of potential new treatments for MNDs, offering hope for improved outcomes and better quality of life for those affected
Raising awareness and supporting research
Motor neurone diseases, including ALS, have a profound impact on individuals, families, and communities worldwide. Raising awareness about these debilitating conditions is crucial for promoting early detection, fostering understanding, and garnering support for research efforts.
Individuals and organisations can contribute to the fight against MNDs in various ways:
- Participating in clinical trials: By enrolling in clinical trials, individuals with MNDs can play a vital role in advancing research and helping to develop new treatments
- Supporting advocacy and awareness campaigns: Engaging with local and national organisations dedicated to MND awareness and research can help raise funds, educate the public, and advocate for improved healthcare and support services
- Volunteering and fundraising: Volunteering time or contributing to fundraising efforts can provide invaluable support to individuals living with MNDs and their families, as well as fuel ongoing research initiatives
By fostering a collaborative and compassionate approach, we can work towards a better understanding of motor neuron diseases, improve the quality of life for those affected, and ultimately strive for effective treatments and potential cures.
Sources
- Motor Neuron Diseases – National Institute of Neurological Disorders and Stroke
- What is ALS – MND?
- Amyotrophic lateral sclerosis (ALS) – Symptoms and causes – Mayo Clinic
- About ALS and Motor Neuron Disease – NEALS
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.