Smoking Cessation Treatments
* Includes Free Private Prescription & Consultation.
† Applies to UK only.

START YOUR TREATMENT TODAY
Available Treatments for Smoking Cessation
SAFE PRESCRIBING
Get Started With the Right Treatment for You
MEDICAL INFORMATION
Smoking Cessation Key Facts

(Current Version)
Smoking is a major health problem impacting on other health conditions such as heart disease, lung cancer, and chronic obstructive pulmonary disease (COPD). According to NICE, there were 474,000 hospital admissions and 79,000 deaths caused by smoking, in 2015-16.
Here, we will take a closer look at the benefits of quitting smoking, effective strategies, local stop-smoking services, and insights into overcoming relapses.
Understanding the challenges of quitting
Those deciding to quit smoking often face challenges:
- Nicotine withdrawal symptoms such as irritability, anxiety, and difficulty concentrating
- Cravings and triggers, such as stress or mood swings
- Slips and relapses
Smoking Cessation strategies, such as quit-smoking medications, can help manage cravings and withdrawal symptoms and improve the chances of quitting.
Benefits of quitting smoking
- A decrease in blood pressure and the risk of heart attacks as well as cancer. Quitting smoking can increase life expectancy by as much as 10 years
- Average smokers save around £38 a week, which adds up to around £2,000 a year
- Improved physical and mental health, improved sense of taste and smell, easier breathing, increased energy levels, reduced anxiety, depression, and stress
- Harmful carbon monoxide levels in your blood will be reduced by half
- Health benefits extend to loved ones, reducing non-smokers exposure to secondhand smoke
Including interventions for tobacco use, changes in diet, and reducing alcohol intake can enhance benefits, further improving outcomes for ex-smokers.
Effective strategies for Smoking Cessation
- Finding personal motivations to quit smoking
- Preparing a quit plan with a quit date and exploring support options like quit-smoking classes, apps, counselling, and medications
- Removing all tobacco products from your home, as well as cleaning thoroughly to remove the smell of tobacco smoke
- Nicotine replacement therapy (NRT) such as nicotine gum, patches, lozenges, inhalers, electronic cigarettes (e-cigarettes) or vaping can help make quitting more bearable
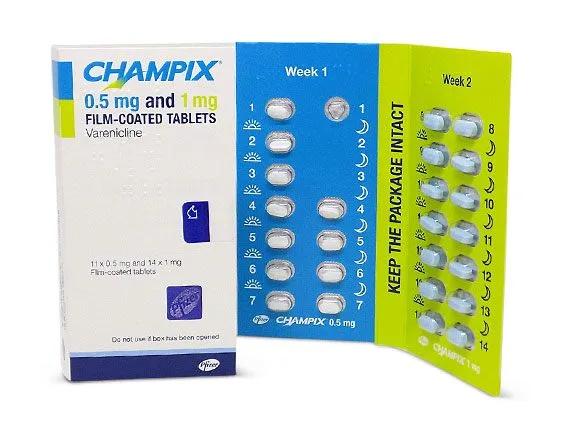
- Prescription medications such as bupropion (Zyban), varenicline and cytisine
- Family, friends and colleagues can help support you with your quit attempt
- Regular exercise can help distract you from cravings and reduce withdrawal symptoms
- Eat well-balanced meals with plenty of fruits, vegetables, whole grains, and lean proteins
- Use delay tactics to distract yourself when you have cravings
- Use healthy substitutes such as carrots or nuts instead of reaching for a cigarette
- Resist the temptation to smoke ‘just one’ cigarette
- Try meditation, yoga, or listening to calming music to relieve stress
- Learn from past attempts to understand what worked and what didn’t
Use resources such as NHS Stop Smoking Services, or Smokefree Smartphone Apps to support your smoke-free life.
Support systems and resources
Resources and support systems include:
- Consulting with a GP, pharmacist, or health visitor in England, Scotland, or Wales
- Digital support tools are useful resources to track your progress and to receive daily support
- Community and online support that can be accessed via phone or video call. The NHS provides 28 days of email support, a Quit Smoking Support Group, and the National Smokefree Helpline
- The American Cancer Society and Smokefree.gov provide tools and guides
These support systems and resources can improve your chances of success in maintaining a smoke-free lifestyle.
Overcoming relapses
Relapses are a common problem when trying to quit smoking. Here are some tips on how to navigate relapses effectively:
- Understanding what led to the relapse. Did you have a stressful day at work, was it a social event with other smokers? Reflecting can provide a learning opportunity. Reflect on the cause and use it as an opportunity
- Identify and manage triggers:
- Practice deep breathing or mindfulness for stress or anxiety
- Change your routine or environment if you normally smoke after meals
- Avoid being around other smokers or prepare with NRT
- Use delay tactics like drinking water or a 10-minute walk if you have the urge to smoke
- Engage with support from family, friends, or support groups
Identify and avoid common triggers, and seek support to address relapses.
Conclusion
As you continue on your journey, it is important to remember that while the process might be challenging, the health benefits are worth it. If you need further support, try NHS Stop Smoking Services and Smokefree Smartphone Apps for additional guidance.
Frequently asked questions about Smoking Cessation
What are the essential steps in a Smoking Cessation intervention?
The essential steps are known as the “5 A’s”: Ask, Advise, Assess, Assist, and Arrange. This helps to identify smokers and provide appropriate interventions.
What does a Smoking Cessation service entail?
Smoking Cessation services provide ongoing behavioural support and the provision of Nicotine Replacement Therapy (NRT). These services are provided by pharmacists who have appropriate training in Smoking Cessation.
What are the 5 R’s related to Smoking Cessation?
The 5 R’s are motivational strategies designed to complement the 5 A’s. They include Relevance, Risk, Rewards, Repetition, and Roadblocks.
What is the most effective method to quit smoking permanently?
The most effective method to quit smoking involves a combination of quit-smoking products such as nicotine patches, lozenges, gum, inhalators, nasal sprays, and medication such as bupropion, as well as enrolling in support programs. Programs should be led by suitably trained professionals in treating tobacco dependence. Options include community stop-smoking groups or in-person or telephone consultations.
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.
Related Articles
OUR CUSTOMERS VIEW
What Customers Love About Our Service
We want everyone to be happy and healthy, that’s what keeps us going. Read what some of them have to say about us.
Medicines Experts
Meet Our Medical Team
We are a broad skilled and passionate group of clinicians with experience of operating in health systems in the United Kingdom & United States. Providing excellent care and advice is at the heart of everything we do. You can read more about our medical team by visiting the medical team page or learn more about how we curate content by visiting our editorial process