Colorectal cancer, also known as colon cancer or rectal cancer, is a type of cancer that originates in the large intestine (colon) or the rectum. This type of cancer develops from precancerous growths called polyps, which can slowly turn into cancerous tumours over time. It is a serious health concern that affects millions of people worldwide and can have devastating consequences if not detected and treated early. Understanding the key risk factors associated with colon cancer is crucial to prevention and early detection.
This article explores the main causes of colon cancer, shedding light on factors that increase a person’s likelihood of developing this disease. From age and family history to lifestyle choices and pre-existing medical conditions, readers will gain valuable insights into the various elements that contribute to colon cancer risk. By learning about these factors, individuals can take proactive steps to protect their health and reduce their chances of developing this potentially life-threatening condition.
Age and family history
Increased risk with age
Colon cancer risk increases as people get older, with most cases diagnosed after the age 50. However, a concerning trend has emerged in recent years. Colorectal cancer diagnoses are rising among individuals under 50, leading to updated screening recommendations. The American Cancer Society advises beginning colorectal cancer screenings at age 45 instead of 50.
Hereditary factors
Family history plays a significant role in colon cancer risk. About one in three people who develop colorectal cancer have family members who have had it. The risk is higher if a first-degree relative (parent, sibling, or child) was diagnosed, especially if they were younger than 50 or if multiple first-degree relatives were affected. People with a family history may need to start colonoscopy screening at 40 or 10 years before their relative’s diagnosis age.
Genetic syndromes
Approximately 5% of colorectal cancer cases are linked to inherited genetic mutations. These hereditary syndromes significantly increase the risk of developing multiple cancers. The most common genetic conditions associated with colon cancer include:
- Lynch Syndrome: Accounting for 2-4% of all colorectal cancers, it’s caused by mutations in DNA mismatch repair genes. Carriers have a 50-80% lifetime risk of developing colorectal cancer
- Familial Adenomatous Polyposis (FAP): This condition causes hundreds to thousands of polyps to develop in the colon and rectum, often starting in adolescence. Without intervention, almost all people with FAP will develop colon cancer by age 40
- MYH-Associated Polyposis (MAP): This autosomal recessive condition presents with features similar to attenuated FAP but without a strong family history
- Hamartomatous Polyposis Syndromes: These rare disorders, including Peutz-Jeghers syndrome, juvenile polyposis, and Cowden syndrome, are associated with a high risk of gastrointestinal malignancy
It’s crucial to talk to a doctor about a family history of colorectal cancer. Genetic testing can help identify mutation carriers and at-risk family members, allowing for more targeted and efficient cancer surveillance strategies.
Lifestyle factors
Diet and nutrition
The Western diet has a significant impact on colorectal cancer risk. This diet, characterised by high consumption of processed foods, sugar, and animal fats, has been linked to an increased incidence of colorectal cancer. Research suggests that processed sugar, particularly high fructose corn syrup, may feed tumour growth. Animal fats, when consumed over long periods, can cause severe chronic inflammation, potentially leading to obesity and type 2 diabetes.
Processed meats such as bacon, salami, and hot dogs have been associated with a higher risk of colorectal cancer. A study in the International Journal of Epidemiology found that individuals consuming red or processed meat four or more times a week had a 20% higher risk of colorectal cancer compared to those who ate it twice a week or less.
On the other hand, plant-based diets rich in fruits, vegetables, and whole grains are associated with a lower risk of colorectal cancer. Fibre-rich vegetables like kale, spinach, and broccoli are particularly beneficial for gastrointestinal health. The Mediterranean diet, with its emphasis on fruits, vegetables, legumes, nuts, and berries, is considered one of the best dietary approaches for reducing colorectal cancer risk.
Physical activity
Physical activity plays a crucial role in preventing colorectal cancer. Studies have shown that regular exercise can prevent approximately 15% of colon cancers. Research indicates that individuals who exercise for at least one hour per week have a lower prevalence of colon polyps and adenomas compared to those who exercise less.
A meta-analysis revealed that physical activity resulted in a 24% decrease in colon cancer risk. The anti-cancer effects of exercise appear to be dose-dependent, with higher levels of activity associated with greater risk reduction. Recreational activities, in particular, have been found to significantly decrease the risk of colorectal cancer.
Obesity
Obesity is a significant risk factor for colorectal cancer. Overweight and obese individuals have about 18% and 32% greater risk of colorectal cancer, respectively, compared to those with normal weight. Excess weight increases insulin and related hormones in the blood, which can encourage cancer growth. Additionally, excess fat creates an environment conducive to inflammation, further contributing to cancer development.
The link between obesity and colorectal cancer risk is complex and is still being studied. However, maintaining a healthy weight is crucial for reducing the risk of colorectal cancer and improving overall health outcomes.
Medical conditions
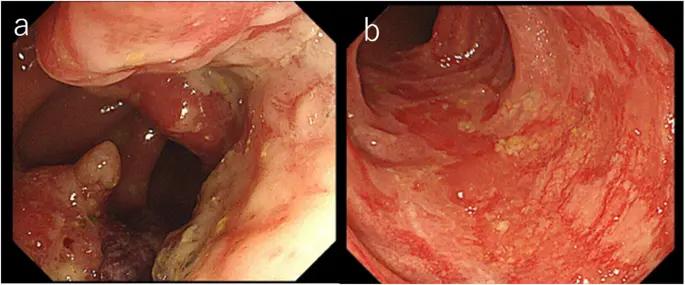
Inflammatory bowel disease
Inflammatory bowel disease (IBD), including ulcerative colitis and Crohn’s disease, significantly increases the risk of colorectal cancer (CRC). Patients with IBD have a two to three-fold higher risk of developing CRC compared to those without chronic colitis. This increased risk is due to long-standing inflammation in the colon, which can lead to abnormal cell growth and eventual cancer development.
The risk of CRC in IBD patients is influenced by several factors:
- Disease duration: Longer disease duration is associated with a higher incidence of CRC
- Age at diagnosis: Younger age at IBD diagnosis is linked with a greater CRC risk
- Extent of disease: Wide disease involvement (>50% of the colonic area affected) is a strong risk factor
- Family history: Having a first-degree relative with CRC doubles the risk
- Presence of primary sclerosing cholangitis (PSC): This condition significantly increases CRC risk in IBD patients
To reduce this risk, regular colonoscopy screenings are crucial. Most guidelines recommend starting surveillance 8-10 years after IBD diagnosis, with follow-up screenings every 1-3 years depending on individual risk factors.
Type 2 diabetes
Type 2 diabetes mellitus (T2DM) has been identified as a risk factor for colorectal cancer. Studies have shown that patients with T2DM have an 18% higher risk of developing CRC compared to those without diabetes. This increased risk is due to several factors:
- Hyperinsulinemia: High insulin levels can promote cancer cell growth
- Insulin-like growth factor (IGF) system: This system plays a role in cell proliferation and inhibition of apoptosis
- Hyperglycaemia: Elevated blood sugar levels can lead to chronic inflammation and oxidative stress
- Obesity-induced inflammation: Adipose tissue dysfunction contributes to a tumour-supporting environment
The association between T2DM and CRC risk appears to be stronger in females and varies with diabetes duration. Interestingly, some diabetes medications, such as metformin, may reduce CRC risk, while others, like sulfonylureas and exogenous insulin, may increase it.
Previous cancer history
Individuals with a history of certain cancers or cancer treatments face an increased risk of developing colorectal cancer. This is particularly true for those who have received radiation therapy to the abdominal or pelvic area. The risk is higher if the radiation treatment is received at a young age or for conditions such as prostate cancer.
Patients with a history of cancer or radiation therapy to the abdominal area may need to start CRC screenings earlier and undergo more frequent screenings. The specific recommendations depend on individual risk factors and should be discussed with a healthcare professional.
Conclusion
Colon cancer is a complex disease influenced by a variety of factors. Age, family history, and genetic syndromes play a significant role in determining an individual’s risk. Lifestyle choices, such as diet and physical activity, also have an impact on the likelihood of developing this disease. To reduce the risk, it’s crucial to maintain a healthy diet, exercise regularly, and keep a healthy weight.
Medical conditions like inflammatory bowel disease and type 2 diabetes can increase the chances of developing colon cancer. Regular screenings are essential to detect and address any potential issues early on. By understanding these risk factors and taking proactive steps, individuals can work to protect their health and lower their risk of colon cancer. It’s always a good idea to talk with a healthcare provider about personal risk factors, treatment options and the best prevention strategies.
Sources
- Colon Cancer: Symptoms, Stages & Treatment
- Colorectal Cancer Risk Factors – Hereditary Colorectal Risk Factors – American Cancer Society
- What Is Colorectal Cancer? – How Does Colorectal Cancer Start? – American Cancer Society
- Colorectal cancer
- Risks and causes of bowel cancer – Cancer Research UK
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.