About 1 in 5 people over 60 in the UK have some degree of peripheral arterial disease. Peripheral arterial disease (PAD) also known as the peripheral vascular disease is a condition that occurs when the arteries in your limbs (usually the legs) become narrowed or blocked. This narrowing or blockage is usually caused by atherosclerosis, a buildup of plaque in the arteries. PAD can lead to some serious health problems, so it’s important to be aware of the symptoms, risk factors and treatments that are available.
What is peripheral artery disease?
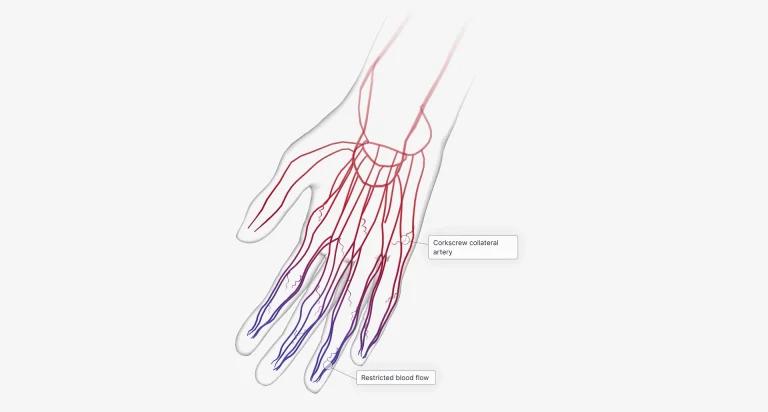
Peripheral arterial disease (PAD) is a condition in which the arteries outside of your heart and brain become narrow or blocked. The most common type is lower-extremity PAD, in which blood flow is reduced to the legs and feet. This happens when plaque, a fatty substance, builds up in your arteries in the lower extremities. Plaque narrows the space inside the artery and reduces blood flow. This is the most common cause of PAD. PAD can lead to serious health problems, including heart attack, coronary artery disease and stroke.
What are the typical symptoms of the peripheral arterial disease?
The most common symptom of PAD is intermittent claudication, which is pain or cramping in your leg muscles, buttocks and hips, that occurs when you walk or exercise. The pain usually goes away with rest. Other symptoms of PAD include:
- Leg numbness or weakness
- Coldness in your lower leg or foot, especially when compared to the other side
- Sores or ulcers on your lower limbs that won’t heal
- Colour changes in your legs or feet
- Poor toenail and fingernail growth
- Hair loss on your legs or feet
If you have any of these symptoms, it’s important to see a doctor so that you can be diagnosed and treated for PAD. Early diagnosis and treatment can help prevent serious health problems down the road. Untreated peripheral arterial disease can lead to serious problems, including gangrene (tissue death) and amputation (removal of a body part).
However, many people with PAD don’t experience any symptoms at all. In some cases, you may dismiss mild leg pain from PAD as a sign of ageing and nothing more. That’s why it’s important to be aware of the other risk factors for PAD (listed below), so you can talk to your doctor about getting tested even if you’re not experiencing any symptoms.
Risk Factors for PAD
There are several risk factors for peripheral artery disease, including:
Smoking
Smoking puts you at higher risk for peripheral arterial disease. Smoking damages the lining of the arteries, making them more susceptible to narrowing or blockages. Second, smoking increases the build-up of plaque in the arteries. Finally, smoking causes inflammation throughout the body, including in the arteries. This inflammation makes it more difficult for blood to flow freely and can contribute to the development of PAD.
High blood pressure (hypertension)
Over time, high blood pressure puts strain on the arteries, causing them to become narrowed and hard. This narrowing makes it difficult for blood to flow through the arteries, which can eventually lead to PAD. In addition to causing PAD, high blood pressure also increases the risk of heart attack and stroke.
High cholesterol
High blood cholesterol is a major risk factor for PAD because it contributes to plaque buildup that collects on artery walls.
Diabetes
There are two main ways that diabetics are at increased risk of developing PAD. First, high levels of blood sugar can damage the blood vessels, making them more susceptible to atherosclerosis. Second, diabetes can cause changes in the nerves that control blood flow. These changes can make it difficult for the arteries to dilate properly, which can further reduce blood flow and lead to PAD.
Family history of cardiovascular disease
Family history is another risk factor for PAD. Cardiovascular disease (CVD) includes all diseases of the heart and blood vessels, such as coronary heart disease, stroke and peripheral artery disease. CVD runs in families, which means that genetics plays a role. If you have a parent or grandparent with CVD, you are more likely to develop the disease yourself. The risk goes up even more if more than one family member has CVD.
Obesity
Obesity can damage the endothelium, which is the inner lining of your arteries. This damage leads to inflammation, which narrows the arteries and reduces blood flow. In addition, fat tissue produces hormones that increase inflammation and make it more difficult for the body to repair damaged arteries. Obesity also makes it more likely that you will develop diabetes, another major risk factor for PAD. Together, these factors can greatly increase your risk of developing this serious condition.
Lack of physical activity
When you don’t move your muscles, they require less blood flow. As a result, the arteries supplying those muscles can become narrower. In addition, lack of physical activity can contribute to other risk factors for PAD, such as obesity, diabetes and high blood pressure.
Age (PAD is more common in people over age 50)
As we get older, our arteries tend to lose some of their flexibility and elasticity. This makes them more susceptible to damage from things like high blood pressure and cholesterol. Over time, this damage can lead to the formation of plaque, which narrows the arteries and limits the flow of blood. In people with peripheral arterial disease, this process is accelerated, it can eventually lead to serious problems like pain, disability, and even amputation.
How is PAD diagnosed?
PAD is diagnosed through a combination of physical examinations and tests. The physical examination may reveal decreased pulses in the affected limb as well as changes in skin colour or temperature.
Tests used to diagnose PAD include an ankle-brachial index (ABI), Doppler waveform analysis, magnetic resonance angiography (MRA) and angiogram.
An ABI is the most common test used to diagnose PAD. It is a non-invasive test that uses a blood pressure cuff and a ultrasound probe to measure blood flow in the arteries. ABI values below 0.9 are considered diagnostic for PAD.
Doppler waveform analysis is another non-invasive test that uses sound waves to measure blood flow in the arteries. MRA is an imaging test that uses magnetic waves and x-rays to create pictures of the arteries.
An angiogram is an invasive test that uses dye injected into an artery to make the artery visible on x-ray images. It is generally only used if other tests are inconclusive or if there is suspicion of severe disease causing blockages of multiple arteries.
What is the best treatment for peripheral artery disease?
The first line of therapy is typically aimed at controlling risk factors such as diabetes, high cholesterol and hypertension. If lifestyle changes are not enough, then medications may be prescribed to improve symptoms and quality of life. If medical management fails to relieve symptoms, interventional procedures such as angioplasty or bypass surgery may be recommended.
Lifestyle
Quitting smoking is one of the most important lifestyle changes you can make if you have PAD. Smoking damages the lining of the arteries, making them more likely to become blocked. Quitting smoking can help to reverse this damage and improve blood flow.
Exercise is another important part of treating PAD. Regular exercise helps to improve circulation and reduce the risk of clots forming in the arteries. Walking, cycling and swimming are all good exercises for people with PAD. However, it’s important to check with your doctor before starting any new exercise programs.
Eating a healthy diet is also important for people with PAD. A diet rich in fruits, vegetables and whole grains can help to improve symptoms and reduce the risk of complications. Avoiding fatty foods, salt and sugar can also help to keep your arteries healthy.
Making these lifestyle changes can be difficult, but they’re essential for treating PAD. Talk to your doctor about what changes you need to make to manage your condition. With time and effort, you can improve your symptoms and reduce your risk of complications from PAD.
Medication
Medications used to treat PAD include:
- Antiplatelet agents: These medications prevent blood cells from sticking together and forming blood clots that can further block arteries. Aspirin is the most commonly used antiplatelet medication. Cilostazol, clopidogrel is another commonly used drug
- Cholesterol-lowering drugs: Statins are medications that reduce the production of LDL (“bad”) cholesterol. By lowering LDL levels, statins can help to slow the progression of PAD
- Vasodilators: These medications work by relaxing the smooth muscle cells in artery walls, which widen the arteries and improves blood flow. Nitroglycerin is the most commonly used vasodilator for treating PAD. While effective, vasodilators can cause side effects such as headache, dizziness and flushing. As a result, they are typically only used on an as-needed basis
Vascular surgery
Angioplasty is a minimally invasive procedure. A long thin tube called a catheter is inserted into an artery in your leg. Then a small balloon at the end of the catheter is inflated to open up the artery. A stent (a small mesh tube) may also be placed in the artery to help keep it open. Bypass surgery is a more invasive procedure that involves taking a healthy blood vessel from another part of the body and using it to create a new path around the blocked artery. Both procedures can relieve symptoms and improve blood flow.
If you think you may be at risk for peripheral arterial disease or if you’re experiencing symptoms like leg pain or numbness it’s important to see your healthcare provider right away. They will be able to order tests to confirm a diagnosis and develop a treatment plan to help reduce your risk of serious complications like amputation or gangrene. With early diagnosis and treatment, you can enjoy a good quality of life despite having PAD.
Sources
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information on this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.