What is pharmacogenomics and what does it mean for your health?

What is Pharmacogenomics?
Genes are sections of DNA (deoxyribonucleic acid) that pass from parents to offspring and contain coded genetic information that ultimately defines our physical and biological traits. Physical traits include hair and eye colour, and height.
People can have different variants of the same gene. These genetic variations can be rare or common. These variations used to be known as mutations; however, since changes in DNA do not always cause disease, it is thought that gene variant is a more accurate term.
Pharmacogenetics studies how a genetic variation in one single gene can affect the individual’s response to a single drug. It essentially envelops the science of drugs (pharmacology) and the study of genes (genomics). Pharmacogenomics is a broader term and refers to how all of the genes (the whole human genome) influence response to drugs. Commonly these terms are often used interchangeably.
Pharmacogenetics allows healthcare providers to tailor medical treatment by prescribing treatments based on a person’s genetic make-up. This is a practice known as precision medicine.
What have my genes got to do with how effective the medications I take are?
Genes not only define physical traits such as hair, eye colour and height, but they also define biological traits such as how our bodies respond to medicines.
Genetic variability can be standard or also rare. A gene variant means there is a slightly different DNA sequence and this can affect the absorption, distribution, metabolism, and elimination (“pharmacogenes”) of medications. The variants can significantly influence an individual’s drug response and consequently the effectiveness of treatment and possible adverse drug reactions or side effects.
Why is Pharmacogenomics important?
Human genome sequencing is well-established in the United States. Clinical screening programs examine genes or variants in unselected populations to identify individuals at increased risk to help prevent future disease or adverse drug outcomes. The uptake of tests in the United Kingdom is low since the services are not yet well established.
When your doctor starts you on a treatment for a particular condition, they will usually prescribe one of several appropriate medicines. The dose and timing of that medicine are usually based on several factors, such as the rate of metabolism and clearance from the body in the average person.
The doctor will typically begin by prescribing a “standard” dose based on factors such as weight, sex and age and then adjust the dose or change the drug over time, depending on the patient’s treatment outcomes or tolerance to that medication.
Some drugs have a narrow therapeutic index, which means that there is only a small difference between the minimum effective concentrations and the minimum toxic concentrations in the blood.
With such drugs, small increases in the dose or blood/serum concentrations could lead to toxic effects. In these instances, the doctor may monitor you with blood tests and the dosages increased or decreased to maintain the drug level in an established “therapeutic” range. If changing the drug dose is not effective in treating or controlling the patient’s condition, or side effects persist, then the patient may be given a different drug and the process is started again.
Genomic testing or pharmacogenetic testing offers a new practical approach to individualise drug therapy for patients based on their genetic make-up, so patients get the dosage right from the start.
Testing people helps predict the way in which they are likely to respond to certain classes of drugs. For certain medications, pharmacogenomic testing is already helping doctors predetermine drugs and doses that have the best chance of achieving the desired therapeutic effect while reducing the likelihood of serious side effects.
What does a Pharmacogenomics test do?
NowPatient offers the UK’s only direct-to-patient Pharmacogenomics (PGx) service, which provides clinicians with genomic information that can help them optimise their drug administration therapy.
We currently offer the test for genetic variants that result in non-extensive Cytochrome P450 2D6 (CYP2D6) and Cytochrome P450 2C19 (CYP2C19) enzyme activity. The tests can determine if you are an NM (normal metaboliser), IM (intermediate metabolise), PM (poor metaboliser) or UR (ultra-rapid metaboliser) of the CYP2D6 and CYP2C19 enzymes.
These enzymes are essential in the metabolism of a range of drugs, some of which include:
- Citalopram
- Clomipramine
- Clopidogrel
- Diazepam
- Omeprazole
- Biguanides
- Olanzapine
- Haloperidol
- Codeine
- Tramadol
- Abacavir
- Oncology drugs
- Breast Cancer drugs
- Cancer treatment drugs
- Other medications to treat some Cancers, Heart Disease, Blood Pressure
What does a Pharmacogenomics test result mean in clinical practice?
Pharmacogenomic test reports give information about an individual’s collection of genetic variants (or genotype) which affects the way an individual metabolises or reacts to medicines in certain ways (phenotype).
The genotype reported may be expressed in two different ways, using star nomenclature or DNA variants. The most common way of reporting is using star nomenclature. This type of report provides the genotypic results using star (*) nomenclature as an abbreviation for known alleles (different versions of a gene) containing different genomic variants. Results are also normally provided as a diplotype, meaning that it includes one maternal and one paternal allele.
The clinical Pharmacogenetics Implementation Consortium (CPIC) was established in 2009 and includes Pharmacogenomics Research Network members and PharmGKB staff. The CPIC guidelines are used to assist clinicians to understand HOW available genetic test results should be used to optimize drug therapy.
CPIC’s purpose is to enhance the clinical implementation of pharmacogenetic tests by creating, curating, and posting freely available, peer-reviewed, evidence-based, updatable, and detailed gene/drug clinical practice guidelines.
Let’s take a real-world example where you are taking certain antidepressant medications and are subsequently determined to be a PM (poor metaboliser) of CYP2C19 then this is what it could mean for you:
- Antidepressant effectiveness is 36% lower
- Antidepressant central nervous system side effects are 43% more intensive
- Gastrointestinal side effects are 22% more intensive
A poor metaboliser (PM) means the CYP2C19 enzyme has very little activity. Poor metabolisers break down some medicines very slowly and are likely to need different doses than normal metabolisers (NM).
If you are taking any medications that are sensitive to CYP2C19 or CYP2D6, you can discuss the results with your GP. This may lead to refining your dose or a change in medication to something more suitable for you and your health condition.
Sources
Medical Disclaimer
NowPatient has taken all reasonable steps to ensure that all material is factually accurate, complete, and current. However, the knowledge and experience of a qualified healthcare professional should always be sought after instead of using the information in this page. Before taking any drug, you should always speak to your doctor or another qualified healthcare provider.
The information provided here about medications is subject to change and is not meant to include all uses, precautions, warnings, directions, drug interactions, allergic reactions, or negative effects. The absence of warnings or other information for a particular medication does not imply that the medication or medication combination is appropriate for all patients or for all possible purposes.
Related Articles
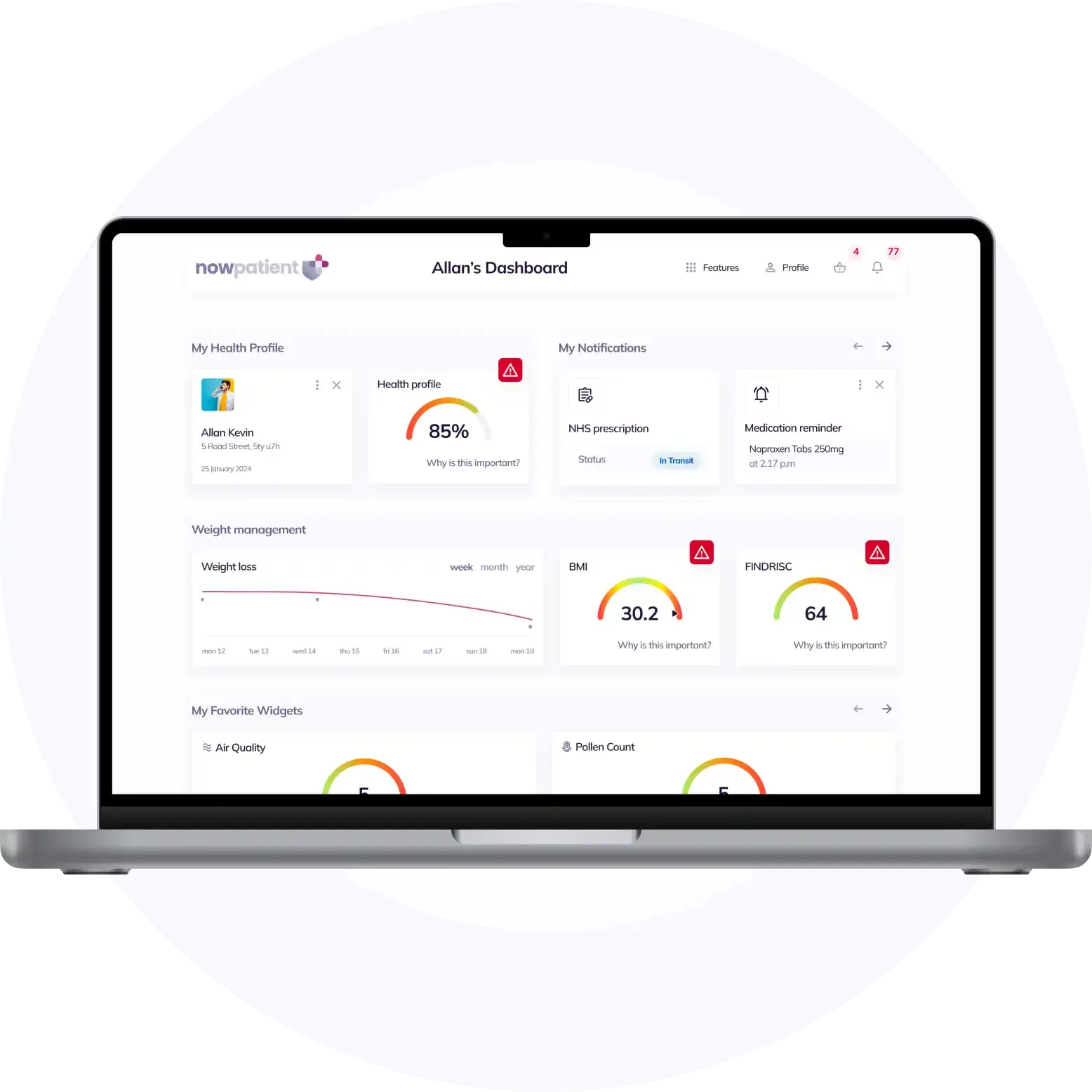
What is NowPatient
Telehealth and Online Pharmacy
NowPatient is a licensed online pharmacy and doctor service that is available around the world. Our service is FREE and packed with valuable features that can benefit your health such as medication reminders, educational blogs, medically approved symptoms checker, UK NHS online pharmacy, private treatment plans, Rx Advantage card, health conditions information, affordable medications options, genetic testing, home test kits, health risks, pollen meter, air quality monitor, weight loss plans, drug savings programs and lots more!
WHY WE BUILT NOWPATIENT
To improve the lives of everyone by making high-quality care accessible and convenient
We are here to improve lives. Our service gives you access to smart features and resources that can help empower you to take control of your health and improve your health outcomes. All this, in one place, for FREE. We strive to bring a fresh perspective to managing health. NowPatient can be accessed by downloading the App or using your web browser.
Download our app today

Can I trust NowPatient
Meet our medical team
We are a passionate group of clinicians and medical writers covering a broad range of specialities with experience operating in health systems in the United Kingdom & United States. Providing excellent care and advice is at the heart of everything we do. You can read more about our medical team by visiting the medical team page or learn more about how we curate content by visiting our editorial process


